Lead is a potent neurotoxin that can cause significant central nervous system dysfunction in both acute and chronic exposures. While paediatric lead encephalopathy is more widely recognised, adult presentations are rare and frequently overlooked. The clinical manifestations often overlap with autoimmune encephalitis (AIE), a leading cause of rapidly progressive neuropsychiatric syndromes, resulting in diagnostic delay and mismanagement (Manuraj et al, 2025; Vaphiades & Carey, 2023). In India, unregulated cosmetics and traditional preparations remain common sources of exposure (Raut et al, 2021).
Globally, sporadic reports of lead encephalopathy linked to occupational or cultural practices highlight its continuing clinical relevance (Patwardhan et al, 2021). This case describes a beautician who developed lead encephalopathy mimicking AIE, underscoring the importance of occupational history, nursing vigilance, and multidisciplinary care.
Case Report
A 41-year-old female beautician presented with a three-month history of progressive cognitive decline, episodic memory lapses, social disinhibition, vivid visual hallucinations, recurrent headaches, and unsteady gait. She also reported transient diplopia, nausea, vomiting, and two episodes of focal seizures with secondary generalisation. On examination, she was alert but disoriented. Bilateral papilledema, myoclonic jerks of the hands, perioral dyskinesias, mild rigidity, and bilateral limb ataxia were observed, while cranial nerves were intact.
Investigations Undertaken
Diagnosis: Lead encephalopathy secondary to chronic occupational exposure to cosmetic products. The rationale was based on neuropsychiatric features mimicking AIE, a negative antibody panel, anaemia, and markedly raised lead levels.
Nursing Management
The patient’s nursing care was guided by the nursing process, focusing on stabilisation, prevention of complications, and safe discharge planning.
Nursing Diagnosis 1: Risk for neurological deterioration related to raised intracranial pressure
Nursing Diagnosis 2: Risk for injury related to recurrent seizures and impaired coordination.
Nursing Diagnosis 3: Imbalanced nutrition related to anaemia and decreased oral intake
Nursing Diagnosis 4: Deficient knowledge regarding occupational hazards
Outcome and Follow-up
With chelation therapy and comprehensive nursing care, the patient showed marked neurological recovery. Cognition and memory improved, hallucinations resolved, seizures were controlled, and gait was normalised. Papilledema subsided, and repeated blood tests confirmed declining lead levels. She returned to her profession with occupational modifications, including protective equipment and improved workplace ventilation, and remained stable on follow-up.
Discussion
Adult lead encephalopathy remains a diagnostic challenge as it often masquerades as autoimmune or metabolic encephalitis (Manuraj et al, 2025; Vaphiades & Carey, 2023). In India, unregulated cosmetics such as sindoor and kajal are important yet underrecognised sources of exposure (Raut et al, 2022). Globally, cases have been reported in association with Ayurvedic medicines, industrial exposure, and opioid adulterants (Schröter, 1991; Suleman et al, 2021).
Our case is unique in highlighting occupational exposure among beauticians, a rarely described high-risk group. The presence of microcytic anaemia and raised intracranial pressure was a diagnostic clue that distinguished this condition from AIE. Radiological findings of basal ganglia hyperintensities are consistent with lead toxicity, though they may overlap with other causes (Patwardhan et al, 2021). Chelation therapy with agents such as CaNaEDTA, BAL, or succimer is effective if initiated early (Rao et al, 2014).
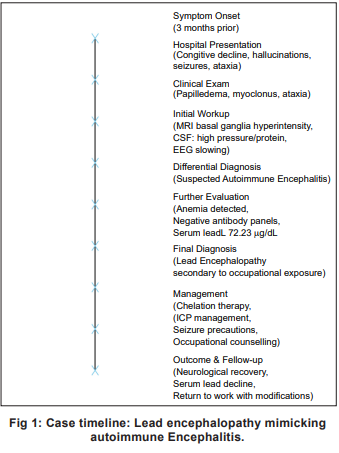
Timeline of clinical presentation, investigations, diagnosis, management, and outcome in a case of lead encephalopathy is shown in Fig 1.
Nurses play a pivotal role in early recognition of atypical features, meticulous neurological surveillance, implementation of seizure and ICP precautions, and occupational counselling, thereby preventing its recurrence and ensuring recovery.
Ethical Consideration
Written informed consent was obtained from the patient for publication of this case report and related clinical details. Institutional ethical approval was not required for a single case report as per policy.
Conclusion
Lead encephalopathy in adults may closely resemble autoimmune encephalitis, risking misdiagnosis and inappropriate immunosuppression. Detailed occupational history, basic haematological evaluation, and nursing vigilance are crucial for timely recognition. Early initiation of chelation therapy facilitates favourable neurological outcomes.
1. Manuraj N, Vijayaraghavan A, Sundaram S, Sukumaran S. Tracing the lead – Lead encephalopathy mimicking autoimmune encephalitis. Ann Indian Acad Neurol 2025; 28(3): 461-63. doi: 10.4103/aian.aian_902_24
2. Vaphiades MS, Carey AR. Take the lead. Surv Ophthalmol 2023; 68(5): 1006-10. doi: 10.1016/j. survophthal.2023.05.005
3. Raut TP, Gholap G, Shaikh S, Mani J, Sanghvi D, Bhatt M. Acute lead encephalopathy secondary to Ayurvedic medication: Two cases with review. Neurol India 2021; 69(5): 1417-20. doi:10.4103/0028-3886.329591
4. Patwardhan A, Atchayaram N, Saini J, Girija MS, Annapureddy J, Alumkadavath M, et al. Lead encephalopathy with distinctive MRI findings. Neurol India 2021; 69(5): 1421-23. doi:10.4103/0028-3886.329588
5. Rao JV, Vengamma B, Naveen T, Naveen V. Lead encephalopathy in adults. J Neurosci Rural Pract 2014; 5(2): 161-63. doi:10.4103/0976-3147.131665
6. Schröter C, Schröter H, Huffmann G. Neurologic and psychiatric manifestations of lead poisoning in adults: Case report and review. Fortschr Neurol Psychiatr 1991; 59(10): 413-24. doi:10.1055/s-2007-1000716
7. Sahu JK, Sharma S, Kamate M, Kumar A, Gulati S, Kabra M, et al. Lead encephalopathy in an infant mimicking a neurometabolic disorder. J Child Neurol 2010; 25(3): 390- 92. doi:10.1177/0883073809338625
8. Shiri R, Ansari M, Ranta M, Falah-Hassani K. Lead poisoning and recurrent abdominal pain. Ind Health 2007; 45(3): 494-96. doi:10.2486/indhealth 45.494
9. Fonte R, Agosti A, Scafa F, Candura SM. Anaemia and abdominal pain due to occupational lead poisoning. Haematologica 2007; 92(2): e13-14. doi:10.3324/ haematol.10951
10. Suleman F, Shoukat K, Arshad A, Khan NU, Sheikh U. Lead encephalopathy in an adult opioid abuser. BMJ Case Rep 2021;14(9): e240977. doi:10.1136/bcr-2020- 240977

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.