Ventilator-Associated Pneumonia (VAP) is a common healthcare-associated infection (HAI) in critically ill patients receiving mechanical ventilation. It typically occurs within 48 hours of intubation and is closely linked to the use of endotracheal tubes (ETTS). Patients with prolonged ventilation, higher illness severity, and underlying lung conditions are at greater risk (Mietto et al, 2013). The better understanding of the pathological events leading to VAP development is made possible by invasive study of lower respiratory tract. However, despite these advances there are no concrete results on altering mortality level and cost of care (Morehead & Pinto, 2000). Prevalence of VAP is often an indicator of the quality of care received by the individual.
New strategies are employed to ensure that there is improvement in secretion drainage and reduction of bacterial colonisation over that ETT that
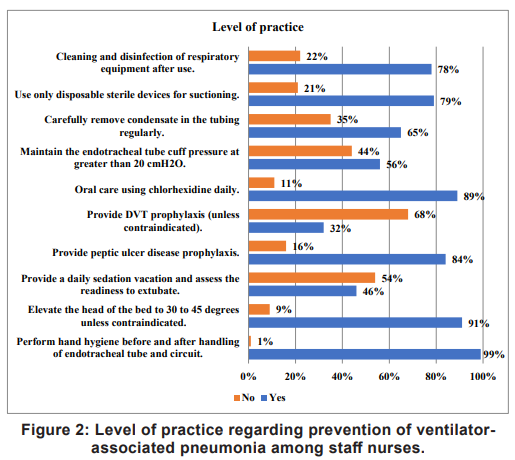
may aid in reducing the occurrence of ventilator- associated events including VAP (Kollef, 2004). Further, there are numerous advances in medical technology that proved to be fundamentally helpful. Nurses across the critical care units have adhered to bundle checklist which includes strategies such as elevation of head and thorax upto 30°, oral care, stress ulcer prophylaxis, maintenance of hand hygiene, etc. (Mietto et al, 2013).
Over the years it has been proven that certain measures can be effective against the prevention of VAP, where we are lacking information regarding these specific interventions. Once we are able to bridge this gap, we will be able to achieve a rather huge milestone and overcome disparities in provision of care and achieve quality health care model (Kollef, 2004). Hence it can be concluded that there is a radical need for further research and clinical studies. Moreover, these studies should also focus on role of nurse regarding prevention of VAP (Mietto et al, 2013).
Despite the availability of evidence-based measures, gaps in nurses' knowledge and practice persist. Bridging this gap is essential to improve patient outcomes and ensure high-quality care. This study aims to assess ICU nurses’ knowledge and practices regarding VAP prevention and examine their association with selected sociodemographic variables.
The Hypotheses: H1 – there is a significant association between the knowledge and practice of ICU nurses in preventing VAP; H2 – there is a significant association between selected demographic variables and the knowledge and practice of ICU nurses concerning VAP prevention.
Review of Literature
In a quasi-experimental study Al-Fazli et al (2024) evaluated the impact of a blended online learning (BOL) training package on nurses’ knowledge and performance in preventing ventilator-associated pneumonia in ICU. A quantitative research design was adopted, with 30 participants each in the intervention and control groups, selected through convenience sampling. Data were collected using a structured knowledge questionnaire and an observational checklist to assess VAP prevention practices. Statistical analysis was conducted using SPSS version 21 at a 5 percent significance level. The results revealed that the mean performance scores in the intervention group increased to 34.1 ± 5.4 and 33.5 ± 5.6, compared to 23.8 ± 4.6 and 24.3 ± 5.7 in the control group. The study concluded that the BOL training method significantly enhanced nurses’ knowledge and performance, suggesting its effectiveness as a valuable tool in VAP prevention education.
Bhandari et al (2021) conducted a descriptive study to evaluate the knowledge of nurses in critical care units regarding VAP prevention bundles at a tertiary cardiac centre in Kathmandu, Nepal. Using a qualitative approach, 57 nurses were selected through purposive sampling, and data were collected via a selfadministered questionnaire. Analysis using SPSS version 21 revealed that while 97.4 percent of nurses had satisfactory knowledge overall, 87.7 percent had not received formal training in VAP or infection control. The study concluded that although general knowledge was satisfactory, gaps remained in understanding VAP definitions and prevention strategies.
Material and Methods
Research approach and design: The quantitative approach with descriptive research design was adopted to fulfil the study objective.
Population and sampling: A total of 100 samples were enrolled using non-probability: purposive sampling from intensive care unit who met the inclusion and exclusion criteria. The sample size was calculated using Raosoft software sample size calculator with a 95 percent confidence level, 5 percent margin of error, and 50 percent response distribution. Based on these parameters, a minimum of 96 samples was required. However, a total of 100 participants were enrolled to ensure adequate representation. Inclusion criteria: (a) Staff nurse`s working in ICU of selected hospital; (b) Nurses who are directly engaged in providing care of ventilator patient; and (c) Nurses who have at least 1year experience in working in ICU. Exclusion criteria: (a) Nurses who are not available at time of data collection; and (b) Nurses who are not willing to participate.
Ethical consideration: After getting approval from the Institutional Ethical Committee, data collection was done. The purpose of the study was explained to participants and their informed consent was obtained; they were given to understand that participation in the study is entirely voluntary; the confidentiality of their responses was assured. ICU nurses were selected using purposive sampling based on inclusion criteria. Participants received an information sheet and completed a structured questionnaire covering demographics and knowledge of VAP. A checklist based on ICD criteria was used to assess their practices regarding VAP prevention. Data were then analysed accordingly.
Tools used: The data was captured by the tool developed by the researcher and validated by the experts which consisted of 3 parts. Part A: Demographic data, Part B: Self-structured questionnaire for assessing knowledge, and Part C: Checklist for assessing practice.
Data analysis: Data was analysed using SPSS software and using descriptive and inferential statistics. Descriptive statistic was used for the demographic data and presented in form of percentage frequency and standard deviation. One sample t-test and Chi square test were applied for categorical variables.
Results
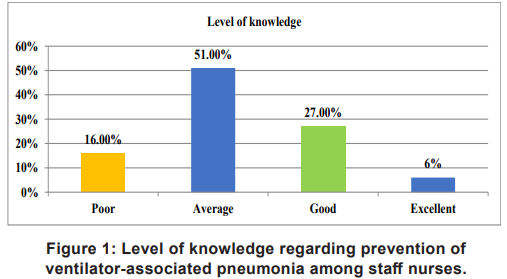
Demographic Characteristics of Nurses The majority of the study participants were female, comprising 83% of the total sample. A significant portion (45%) belonged to the 22–26-year age group, indicating a younger demographic. In terms of educational background, 69 percent of the participants held a Diploma in General Nursing and Midwifery (DGNM). Regarding professional experience, 35 percent had between 0 to 2 years of work experience. When it came to clinical postings, 34 percent reported having worked in a medical ICU. Further, 77 percent of the participants had previously received training related to VAP. As for sources of information, the most commonly reported were books, cited by 46 percent of the participants. Assessment of level of knowledge regarding prevention of ventilator-associated pneumonia among staff nurses Figure 1 illustrates the distribution of knowledge levels among 100 staff nurses concerning the prevention of VAP. The findings indicate that 16 percent of the nurses had poor knowledge, 51 percent had an average level of knowledge, 27 percent displayed good knowledge, and only 6 percent demonstrated excellent knowledge related to VAP prevention. Assessment of level of practice regarding prevention of ventilator associated pneumonia among staff nurse
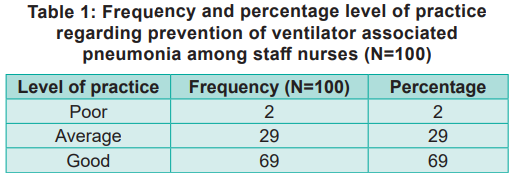
Table 1 provides insight into the practice levels among staff nurses (N=100) concerning the prevention of VAP. Results indicate that 2 percent of participants exhibited poor practice, 29 percent demonstrated average practice, and a significant majority of 69 percent displayed good practice in implementing preventive measures for VAP.
Assessment for correlation between knowledge and practice
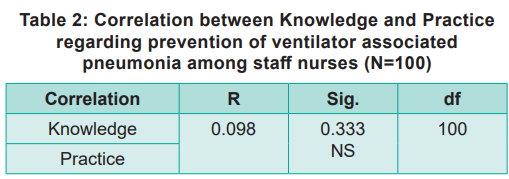
The results of the Pearson correlation indicated that there is a non-significant weak positive relationship between knowledge and practice (r= 0.098, p = 0.333) (Table 2). Thus, the research hypothesis H1 is accepted.
Association of knowledge and practice with knowledge and practice
The analysis revealed a significant association between the area of working and knowledge regarding VAP prevention, indicating that nurses’ work settings influence their understanding. Other demographic factors viz gender, age, qualification, work experience, previous exposure, and sources of information showed no significant association with knowledge. In terms of practice, both qualification and area of working were significantly associated, suggesting their influence on VAP prevention practices. However, variables like gender, age, work experience, previous exposure, and information sources did not show significant associations. Thus, the research hypothesis H2 is accepted for variables that demonstrated significant associations with practice.
Discussion
The findings of this study underscore the critical role of continuous education and hands-on training in improving ICU nurses’ knowledge and practice related to the prevention of ventilatorassociated pneumonia. Drawing upon Maslow’s Hierarchy of Needs, which places physiological needs, such as oxygen at the foundation of human survival, the relevance of optimal respiratory care in critical settings becomes evident. Ensuring effective prevention of VAP, therefore, is not only a clinical necessity but also a fundamental aspect of preserving life.
In the present study, although a majority of nurses (69%) demonstrated good practices in VAP prevention, only 6 percent exhibited excellent knowledge, with most participants falling into the average knowledge category (51%). This disparity between knowledge and practice emphasises the need for targeted educational interventions to bridge this gap. The results revealed a weak positive correlation between knowledge and practice (r = 0.098, p = 0.333), suggesting that enhanced knowledge alone may not directly translate into improved practice without appropriate training reinforcement. These findings are supported by a similar study by Kapoor (2017) at Government Medical College Hospitals in Jammu, where knowledge levels among ICU nurses also varied significantly, with only a small percentage displaying excellent knowledge. In our sample, the majority of participants were female, aged between 22 and 26, with a DGNM qualification and less than two years of ICU experience. Significant associations were observed between area of work and knowledge, as well as between qualification and practice, highlighting the influence of contextual factors onclinical competency. The study highlights an urgent need for structured educational programmes such as lectures, seminars, and simulation-based training to improve both theoretical knowledge and practical skills in VAP prevention. Enhancing these competencies is vital to ensure the delivery of high-quality, evidence-based care and to reduce preventable ICU complications.
Nursing Implications
Limitations:
The study was confined to patients who were on ventilator support only; it focused solely on assessing knowledge and practice, excluding the evaluation of nurses’ attitudes towards the care of ventilated patients in relation to VAP. Participation was limited to nurses who were present during the data collection period. The study included only those nurses with a minimum of one year of ICU experience.
Recommendations
Acknowledgement:
The authors thank the nursing staff of the Intensive Care Unit for their willingness to participate in the study. Their cooperation and openness provided essential data that enriched this research. The literature and previous research studies provided a foundation for this work.
Conclusion
There was a clear disparity between ICU nurses’ knowledge and practice in preventing ventilatorassociated pneumonia VAP. Although most nurses demonstrated good practice, limited knowledge levels highlight the need for ongoing education. The weak positive correlation between knowledge and practice suggests that theoretical understanding must be supported by practical training. Factors like work area and qualifications significantly influenced competency. To enhance care quality, both cognitive and clinical skills should be reinforced through structured programmes such as seminars, lectures, and simulation-based training. Continuous professional development is essential to reduce complications, improve outcomes, and promote a culture of safety in critical care settings.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.