Ensuring access to human milk for all infants has the potential to save countless lives, especially vulnerable neonates, such as those born low-birth weight or pre-mature. Yet many do not have access to their own mother’s milk in the first critical hours or days of life. For such infants, the provision of donor human milk (DHM) is recommended as superior to formula food (PATH, 2019). In India, 30 to 50 percent of vulnerable babies are admitted to the Neonatal Intensive Care Units (NICU), and 10 to 20 percent of term (healthy) babies do not have access to Mother’s Own Milk (MOM) (Sachdeva et al, 2019). According to the National Family Health Survey, as many as 36 percent of the newborns in India do not receive their mother’s milk for reasons such as the mother’s illness, death, abandonment, or delay in milk production, leaving them vulnerable, especially if they are born prematurely. Some mothers also use formula products to feed their babies for medical or non-medical reasons (NFHS, 2023).
Donor Human Milk made available through Human Milk Banks (HMB) is recommended as the next best alternative when MOM is not available (Haiden & Ziegler, 2017; Lawrence & Lawrence, 2012). DHM is human milk produced and collected in excess for an infant’s current and future needs, donated by a mother to an HMB for use by a recipient infant that is not the mother’s infant (Israel-Ballard et al, 2024). The common reasons for donating excess milk to other babies include a feeling of kindness, sisterhood, happiness, satisfaction and belief that mother’s milk has no substitute. Risk of infection to their child, loss of affection for the child, safety concern, loss of milk nutrients, lack of knowledge, motivation, and cumbersome donation process deterred donating breast milk. Home to milk bank distance and easy availability of formula milk between also decreases the willingness to donate or receive milk (Mantri et al, 2022).
When possible, the WHO recommends feeding donor human milk (DHM) obtained from a human milk banking facility for pre-term or low birth weight infants (WHO 2011, 2022). The revised BFHI guidelines of 2018 and 2020 emphasise the need for and use of DHM for vulnerable infants as the foremost choice to meet the exclusive human milk diet (Krishnan et al, 2023). DHM can benefit five million babies annually in India. Human milk in the form of MOM, wet nursing, and DHM is of utmost importance to the survival and development of premature neonates and should be available in adequate quantities for vulnerable newborns. In many developing countries, DHM is not generally available or accepted. Family customs and beliefs play a big role in donating or utilising such milk. Maternal protective instinct also constrains the willingness to utilise DHM (WHO 2011, 2022). In a survey of 16 HMBS in India, it was observed that only a quarter of mothers delivering in hospitals donate milk, and the median annual collection was to the tune of 382 L (range 30–1085 L). The gap between human milk demand and supply is wide and unfulfilled (Sivanandan et al, 2023).
Educating mothers during pregnancy and nursing can foster a strong belief in the value of breastfeeding and inform them about the reasons for donating excess milk. Promoting and educating health staff and professionals, could encourage human milk donors (Doshmangir et al, 2019). The interventions in this regard should be targetted to improve voluntary human milk donation (Sachdeva et al, 2019) and must be incorporated early during the antenatal check-up period for creating awareness, acceptance and utilisation of DHM, and for Social Behaviour Communication Change (Patel et al, 2023). This study aimed to promote awareness among antenatal mothers towards voluntary human milk donation.
Objectives
This study was conducted to (a) Assess the knowledge and attitude of antenatal mothers regarding human milk banking; (b) Analyse the association between knowledge and attitude regarding human milk banking and selected variables; and (c) Find the correlation between knowledge and attitude regarding human milk banking among antenatal mothers.
Methods & Materials
A prospective descriptive research design was used in this study conducted in Gandhi Hospital, Secunderabad, a multi-super-speciality hospital with an operational bed strength of 2200. The MCH block consists of 250 beds. This study was done at the antenatal OPD, which has a footfall of 2500 per month. Study variables were: age, education, occupation, income, gravida, history of donation or receipt of human milk ever, source of information, knowledge and attitude on HMB among antenatal mothers. Samples were antenatal mothers attending at antenatal OPD at Gandhi Hospital. Sample size was calculated, assuming a 95 percent CI with 10 percent margin of error and 50 percent precision, the required sample size was 97, considered as 100, to ensure statistical validity and for fairaccurate estimation of the knowledge and attitudes regarding human milk banking. Purposive sampling technique was used for inclusion of antenatal mothers attending OPD, in their 2nd or 3rd trimester, who understand and speak Telugu/English and/ or Hindi. Antenatal mothers with co-morbidities that contraindicate breast milk donation were excluded from the sampling.
Data collection:
The principal investigator trained four research assistants to collect the data by using a structured questionnaire and an attitude scale by interviewing and questionin
The study tool:
It consisted of two parts. Part A was developed to collect sample characteristics of age, education, occupation, income, gravida, H/O donation or receipt of human milk and source of information. Part B was a questionnaire of 20 questions with four multiple-choice options, with a score of 20. The attitude was measured using a 5-point Likert scale consisting of 10 statements, four were positive statements and six were negative statements. Negative statements were reverse-scored, the maximum score was 50. Higher the score, the better the knowledge and attitude regarding HMB. Both tools were validated by the experts in the field of midwifery and child health nursing.
The pilot study was conducted on 16 August 2024 at the antenatal OPD, Gandhi Hospital, Secunderabad, after getting the formal permission from the hospital authorities. Data was collected from 10 antenatal mothers who fulfilled the sample criteria.
Cronbach’s alpha was used to check the internal consistency for reliability, and the obtained values for the questionnaire and attitude scale were 0.701 & 0.831, respectively. Data collection was done from 19 to 23 August 2024 at the antenatal OPD, Gandhi Hospital, Secunderabad through interviews from antenatal mothers after obtaining their consent. SPSS version 24 was used for analysis. Demographic variables, knowledge and attitude scores were computed using mean, SD and percentages. The chi-square test was used to find the association between the demographic variables and knowledge and attitudes. Pearson’s correlation was used to find the relationship between knowledge and attitudes. p value of 0.05 was considered as statistically significant.
Results
A total of 100 antenatal mothers were recruited for the study. All the mothers were able to respond to the questionnaire and attitude scale freely. The results were analysed by using descriptive and inferential statistics.
Table 1 describes the relationship between age, education, occupation, and income and the knowledge scores of antenatal mothers regarding HMB. The knowledge scores are divided into three categories: ≤7, 8-13, and >14. None of these variables has a statistically significant relationship (p> 0.05) with the knowledge scores of antenatal mothers regarding HMB.
Table 1: Distribution and association of knowledge scores of mothers according to demographic data (N=100)
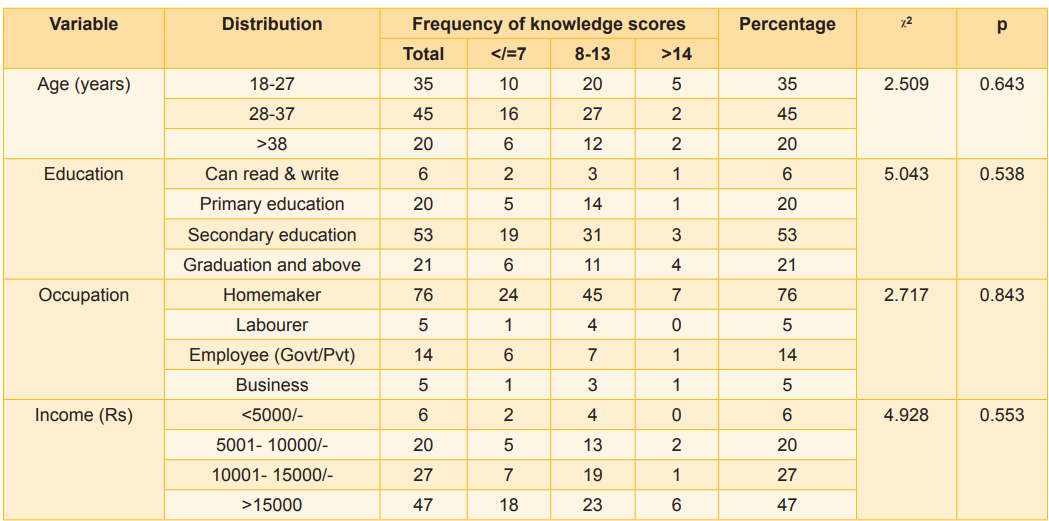
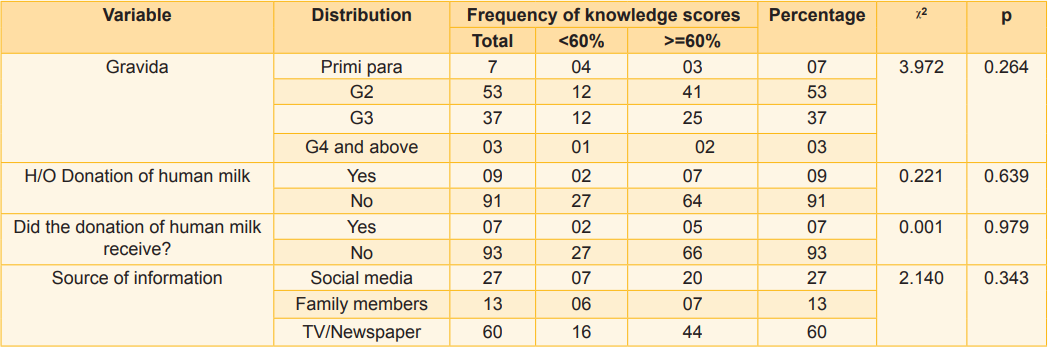
Table 2 depicts the relationship between gravida, history of donating or receiving DHM and sources of information regarding HMB and the knowledge scores of antenatal mothers regarding HMB. The analysis shows that none of the variables have a statistically significant relationship (p>0.05) with the knowledge scores of the antenatal mothers regarding HMB. But it is important to note that 60 percent of mothers do not have any source of information regarding HMB.
Table 2: Distribution and association of knowledge scores of mothers according to demographic data (N=100)
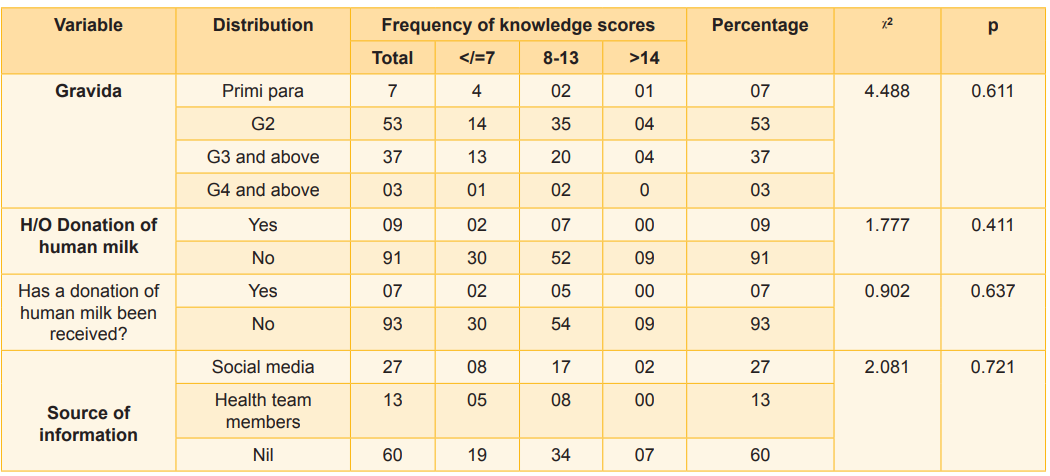
Figure 1: Mean and standard deviation of knowledge and attitude scores
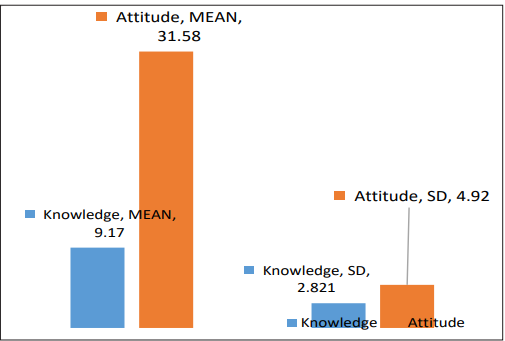
Table 3 presents the relationship between age, education, occupation, and income and the attitude scores of antenatal mothers regarding HMB. The attitude scores are categorised into two groups: those scoring below or above 60. The analysis shows that none of the selected variables has a statistically significant relationship (p > 0.05) with the attitude scores of the antenatal mothers regarding HMB. While age appears to be close to the threshold for significance, it still does not meet the standard criteria for statistical significance.
Relationship between certain variables and the attitude scores of antenatal mothers regarding HMB shows that none of the variables, i.e., gravida, history of milk donation, receiving donated milk, or the source of information, have a statistically significant relationship (p > 0.05) with the attitude scores of the antenatal mothers (Table 4). Correlation between the knowledge and attitude of antenatal mothers regarding HMB was tested by Pearson’s correlation coefficient. There was a significantly positive correlation between knowledge and attitude of antenatal mothers (r = 0.204, p= 0.042).
Table 3: Distribution and association of attitude scores of mothers according to demographic data (N=100)
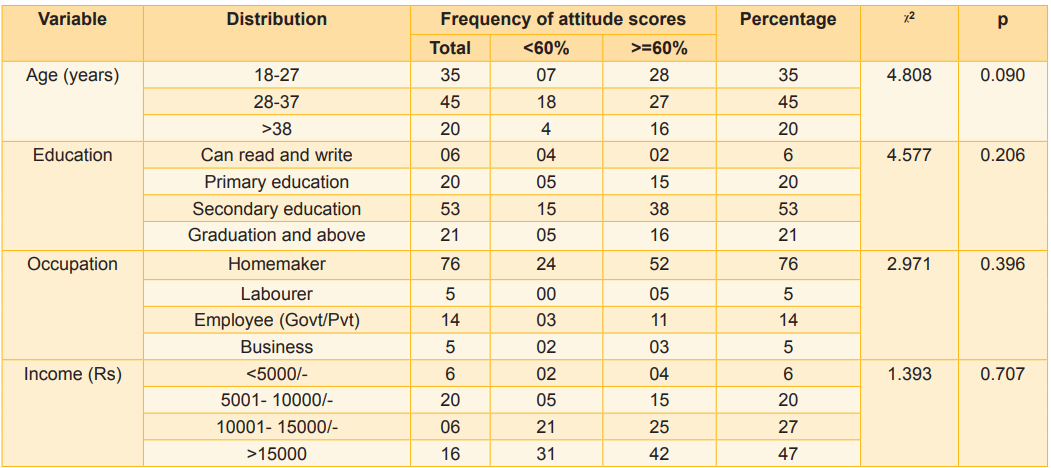
Table 4: Distribution and association of attitude scores of mothers according to demographic data (N=100)
Discussion
The present prospective descriptive design study was conducted on antenatal mothers attending antenatal OPD at Gandhi Hospital, Secunderabad to create awareness among potential future donors of human milk, through a pamphlet in Telugu. The obtained mean knowledge score was 9.17 ± SD 2.821, indicating that the majority of mothers had average and below average scores of knowledges on HMB. These findings are consistent with previous studies in Tamil Nadu (Padmapriya & Snega, 2022) and Punjab (Kaur, Jain, Kansal, 2022). There was no significant association of knowledge of antenatal mothers with selected demographic variables (p > 0.05) in the our study, which is consistent with those of Philomena Fernandes & Sabitha Nayak. Much literature is available on the knowledge and attitudes of post-natal mothers on DHM and HMB, which also shows that mothers lack knowledge on this vital topic (Kaur et al, 2019; Aparna & Padmaja, et al 2021; Mankar & Mourya, 2018; Smitha et al, 2021; Sheela & Shashikala, 2020).
As for the attitude of mothers on HMB, majority of them have a favourable attitude towards it. The obtained mean attitude score in the present study is 31.58 ± SD 4.92, showing that most of the mothers had favourable attitudes towards HMB. None of the selected variables had a statistically significant relationship with the attitude scores of the antenatal mothers regarding HMB. However, a slight tilt in the statistical significance of a favourable attitude towards HMB was noticed in younger mothers when compared to older mothers. These findings are consistent with those of Mankar & Mourya (2018). There was a significant positive correlation between the knowledge and attitude of antenatal mothers. This was consistent with the findings of Tahasildar & Salimath (2021) and Sheela Shasikala, 2020).
Knowledge and awareness regarding HMB can influence and drive mothers to contribute to the noble cause of breast milk donation to the HMB. This study found that most antenatal mothers had no experience as human milk donors or recipients, which could be attributed to a lack of information.
Recommendations
Health authorities, health care professionals, NGOS, and the government shall be proactive in creating awareness among the public on breast milk benefits and voluntary breast milk donation; policy-making authorities shall invest in attracting voluntary human milk donors; the number of dedicated lactation counsellors to be increased as per the load at facilities. needs to be increased. Capacities of staff to be strengthened on HMB to strengthen the capacities of the staff and relevant Information, Education, and Communication (IEC) material in local languages to be displayed in health facilities.
Conclusion
The gap between human milk demand and supply is wide and unfulfilled. This indicates the need for sustained awareness activities regarding HMB among antenatal mothers who would be the prospective donors.
1. PATH. Strengthening Human Milk Banking: A Resource Toolkit for Establishing and Integrating Human Milk Banks, 2019. www.path.org/hmb-toolkit
2. Sachdeva RC, Mondkar J, Shanbhag S, Sinha MM, Khan A, Dasgupta R. A landscape analysis of human milk banks in India. Indian Pediatr 2019 Aug; 56 (8): 663-68. https:// www.indianpediatrics.net/aug2019/aug-663-668
3. Union Health Ministry releases NFHS-5, Phase II Findings 2023. https://www.pib.gov.in/www.pib.gov.in/ Pressreleaseshare.aspx?PRID=177453
4. Haiden N, Ziegler E. Human milk banking. Ann Nutr Metab 2017; 69 (2): 7-15. https://karger.com/anm/article/69/ Suppl.%202/7/42289/Human-Milk-Banking
5. Lawrence Ruth A, Lawrence Robert M. Breastfeeding, 9th edn, 2012. https://www. us.elsevierhealth.com/breastfeeding-9780323680134. html?srsltid=AfmBOoqs09tCjCEa5vdU1_ OxoAA8kMr8YIje2T_F-gBfbKY_UHr7SrxT
6. Israel-Ballard K, LaRose E, Mansen K. The global status of human milk banking. Matern Child Nutr 2024 Jun 20; Suppl 4: e13592. doi: 10.1111/mcn.13592. Epub PMID: 38318679; PMCID: PMC11184569
7. Mantri N, Goel AD, Joshi NK, Bhardwaj P, Gautam V, Gupta MK. Challenges in the implementation of mother milk banks in Rajasthan: A situational analysis. J Mother Child. 2022; 25 (2):86-94. doi: 10.34763. 20212502.d-21- 00009. PMID: 34842395; PMCID: PMC8976586
8. World Health Organisation, United Nations Children’s Fund (UNICEF). 2018 Implementation Guidance: Protecting, Promoting and Supporting Breastfeeding in Facilities Providing Maternity and Newborn Services: The Revised Baby-Friendly Hospital Initiative. World Health Organisation, https://www.who.int/publications/i/ item/9789241513807
9. Krishnan JB, Dhyani Vijayshree, Swamy RS, Gudi Nachiket. A scoping review of interventions to promote voluntary donation of human breast milk in India. Clinical Epidemiology and Global Health 2023; 24 (10): 101449 https://www.researchgate.net/publication/375392569_A_ scoping_review_of_interventions_to_promote_ voluntary_donation_of_human_breast_milk_in_India
10. Sivanandan S, Bethou A, Jebakani S, Calevanane V, Puskaralochanan D. A quality improvement project to improve voluntary milk donation in a human milk bank in South India. Medical Journal Armed Forces India 2023; 79(5): 565-71 https://doi.org/10.1016/j.mjafi.2020.12.015
11. Doshmangir L, Naghshi M, Roghayeh Khabiri. Factors influencing donations to human milk bank: A systematic review of facilitators and barriers. Breastfeeding Medicine 2019 Jun; 14 (5): 298-306. DOI: 10.1089/bfm.2019.0002
12. Patel N, Sumaraj P, Sumaraj P, Gabler T, Grieve A, Naidoo P, et al. Knowledge of breastfeeding and human milk banks amongst mothers at Chris Hani Baragwanath Academic Hospital: A descriptive study. Journal of Clinical Medicine 2023; 5 (1): 25-30
13. Padmapriya D, Snega R. A comparative study to assess the level of knowledge on human milk bank among antenatal mothers at selected urban and rural areas. International Journal of Research in Pharmaceutical Sciences 2020;11(3): 3473-77
15. Kaur H, Maninderjeet K. Raghuvanshi S. Knowledge and attitude of Indian parous women toward human milk banking. Indian Journal of Community Medicine 2019; 44 (2): 175-76. DOI: 10.4103/ijcm.IJCM 377_18
16. Kaur P, Jain S, Kansal N. A study on assessment of knowledge regarding human milk banking among mothers. International Journal of Clinical Obstetrics and Gynaecology 2022: 6 (2): 99-104
17. Aparna P, Padmaja A. Effectiveness of structured teaching programme on knowledge regarding human milk banking among mothers of infants at selected villages of Baireddipalle, Chittoor, IJCRT 2021; 2101089 International Journal of Creative Research Thoughts 2021 Jan; 9(1): 738-49. ISSN: 2320-2882
18. Mankar Ashwini, Mourya Archana. A study on knowledge and attitude regarding human milk banking among postnatal mothers in selected hospitals. International Journal of Science and Research 2018; 7(10): 352-56. ISSN: 2319-7064
19. Smitha Rani S, Devika AK, Lekshmi V. A study to assess the effectiveness of structured teaching programme on human milk banking among adolescents from selected colleges of Thiruvananthapuram. International Journal of Science and Research 2021; 10 (11): 877-79. ISSN: 2319- 7064 SJIF (2020): 7.803
20. Sheela J, Shasikala V. Knowledge and attitude of postnatal mothers on human milk banking. International Journal of Science and Healthcare Research 2020; 5(4): 135-41. ISSN: 2455-87
21. Tahasildar HA, Salimath GB. Mothers’ knowledge and attitude on the feeding of banked human milk among infants, with a view to developing an information booklet. Indian Journal of Health Sciences and Biomedical Research 2021; 14 (2): 211-17. DOI: 10.4103/kleuhsj. kleuhsj_123_20

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.