Cancer patients frequently encounter periods of emotional distress at various stages of their illness journey (Bultz & Johansen, 2011). Distress is considered the ‘sixth vital sign’ in cancer care, and routine screening practices often adhere to guidelines established by the National Comprehensive Cancer Network (Holland & Alici, 2010). The American College of Surgeons’ Commission on Cancer introduced new accreditation standards for patient-centred care mandate that all patients undergo distress screening, requiring an appropriate clinical response to those identified as experiencing distress (Zebrack et al, 2017). If psychosocial distress is not addressed, it can disrupt treatment processes, negatively impacting the disease’s progression and overall patient outcomes (Jacobsen et al, 2005). Timely identification and treatment of distress related to cancer can enhance patient care, foster better communication between providers and patients, and support the effective use of the healthcare team, all essential elements for achieving the best possible patient outcomes (Mitchell et al, 2013).
Cancer is not just a physical illness but also a psychological challenge. A diagnosis of cancer can lead to a range of emotional responses, including shock, denial, fear, anxiety, depression, and hopelessness, all of which can significantly affect a patient’s quality of life and treatment outcomes. Family members, too, often experience stress, anxiety, and emotional turmoil when a loved one is diagnosed with cncer. Coping strategies and support mechanisms are critical to managing these psychological impacts.
This paper aims to examine the psychological effects of a cancer diagnosis on patients and their families, assess the coping strategies employed, and evaluate the effectiveness of various support systems.
Need of the study: Cancer continues to be a major health concern worldwide, not only due to its physical implications but also because of the profound psychological distress it imposes on both patients and their families. A diagnosis of cancer often triggers a range of emotional responses, including fear, anxiety, depression, and a sense of helplessness. These psychological reactions can significantly interfere with the treatment process, delay recovery, and diminish the patient’s overall quality of life. Family members, who frequently take on caregiving responsibilities, are affected emotionally and psychologically. They experience high levels of stress, financial strain, and emotional exhaustion. Despite this, psychological care for both patients and caregivers remains insufficiently integrated into routine cancer treatment, particularly in resource-limited healthcare settings.
This study highlights the urgent need for comprehensive psychological support in cancer care. By identifying the most common emotional challenges, assessing coping mechanisms, and evaluating the effectiveness of support systems such as counselling and support groups, the research provides critical insights into improving emotional well-being and enhancing patient outcomes. It also emphasises the crucial role of nurses and healthcare providers in addressing the psychological aspects of cancer care.
Objectives
The following were the objectives set out for the study:
Review of Literature
Many studies have highlighted the prevalence of psychological distress in cancer patients and their families. Ramasubbu et al (2019) reported higher levels of distress, partly due to limited access to mental health resources and the stigma surrounding mental health and cancer. This lack of integrated psycho-oncology care often leaves psychological symptoms unaddressed, exacerbating the mental health burden on patients and families.
Mitchell et al (2013) found that depression and anxiety are common among cancer survivors and their caregivers, with many reporting higher levels of psychological distress compared to healthy controls. Linden et al (2012) explored the variations in anxiety and depression rates across cancer types, genders, and ages, emphasising the importance of personalised psychological interventions.
Northouse et al (2010) conducted a metaanalysis of interventions for family caregivers, demonstrating the positive impact of tailored support programmes on caregivers’ psychological health. In their study Chambers et al (2012) discussed unmet emotional needs in patients and families contacting cancer helplines.
Methodology
This study was conducted using both quantitative and qualitative approaches. The quantitative phase was conducted in the form of a crosssectional survey, while the qualitative phase was conducted using in-depth one to one interview. A total of 100 participants (50 cancer patients and 50 family members) were recruited from a major cancer treatment centre using purposive sampling. The data collection methods included:
Surveys: Participants completed a psychological well-being survey using the NCCN Distress Thermometer and problem checklist (henceforth called as NCCN-DT) which consists of a singleitem, 11-point Likert scale that is represented in the form of a thermometer that ranges from 0 (no distress) to 10 (extreme distress) along with a 43-item problem checklist, consisting of practical, family, emotional, spiritual-religious or physical problems. Level of distress (range): No distress (0), Mild distress (1–3), Moderate distress (4–6), Severe distress (7–9), Extreme distress (10).
Interviews: Semi-structured interviews were conducted with 20 patients and 20 family members to explore their coping mechanisms and the support they received.
Results
Quantitative data from the surveys were analysed using statistical tools, while qualitative data from the interviews were thematically analysed to identify patterns in coping strategies and support mechanisms.
The quantitative data collected through surveys were analysed using descriptive statistics. The mean depressive score for patients was found to be 4 on a scale of 10, indicating moderate levels of depression. Similarly, depression scores averaged at 3, suggesting significant depressive symptoms for family members.
Correlation analysis indicated a significant negative correlation (r = -0.65, p < 0.01) between the use of active coping strategies and levels of psychological distress, confirming that active coping leads to better emotional outcomes. The results concluded as:
Psychological impact on patients:
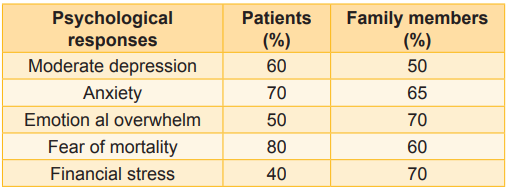
Data analysis revealed that 60 percent of cancer patients experienced moderate depression during the initial stages following their diagnosis (Table 1). Common psychological reactions among patients included fear of mortality, concern about the treatment process, and uncertainty about their future.
Psychological impact on families:
Families of cancer patients also showed significant emotional distress. Around 70 percent of family members reported feeling emotionally overwhelmed and 50 percent experiencing symptoms of depression (Table 2). Many family members expressed concerns about the burden of caregiving and financial instability.
Correlation analysis indicated a significant negative correlation (r = -0.65, p < 0.01) between the use of active coping strategies and levels of psychological distress, confirming that active coping leads to better emotional outcomes.
Table 1: Sociodemographic characteristics of participants
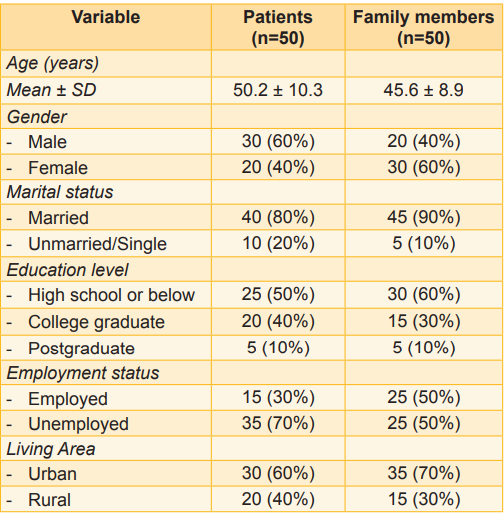
Table 2: Psychological impact of cancer diagnosis
The thematic analysis of interview data revealed common themes, including fear of the unknown, struggles with treatment side effects, and the importance of family support. Patients often expressed feelings of isolation, but those who engaged in social activities or sought counselling reported better emotional adjustment.
Coping strategies for patients:
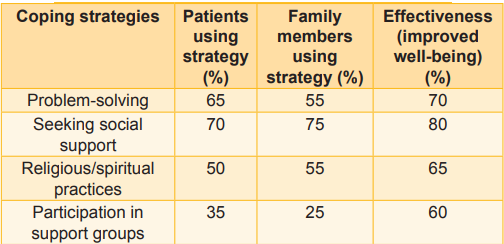
Quantitative analysis of the survey data indicated that patients who employed active coping strategies, such as problem-solving and seeking social support, reported lower levels of psychological distress (Table 3). Specifically, 65 percent of patients who engaged in active problem-solving techniques showed significant reductions in emotional instability levels, while 70 percent of those who sought emotional support from family and friends reported a better sense of psychological wellbeing.
Coping strategies for families:
Families primarily relied on social support, with 75 percent indicating that strong familial and community support helped them manage their emotional burden. Religious and spiritual practices were also frequently used as coping mechanisms, with 55 percent of family members reporting that these practices provided comfort and hope during challenging times.
Table 3: Coping strategies and effectiveness
Effectiveness of support mechanisms:
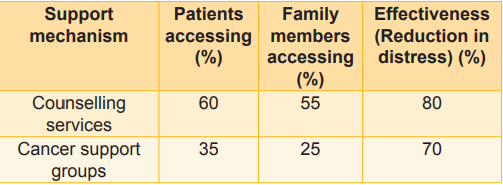
Counselling and psychological support - Of the 100 participants, 60 percent of patients and 55 percent of family members had accessed counselling services. Counselling was associated with significant reductions in reported depression, with 80 percent of those who received counselling reporting improved psychological well-being (Table 4).
Participation in cancer support groups was also highly effective. Patients who attended support groups regularly (35%) reported a marked improvement in emotional coping, highlighting the benefits of shared experiences and mutual support.
Table 4: Access to support mechanisms
Discussion
The results of this study highlight the profound psychological impact of a cancer diagnosis on both patients and their families. The data show that anxiety and depression are the most common psychological responses among both groups. These findings align with those of (Normen et al, 2021), which has shown that emotional distress is prevalent among cancer patients and their caregivers.
Coping strategies play a crucial role in managing these psychological effects. Active coping mechanisms, particularly problem-solving and seeking social support, were found to be the most effective in reducing psychological distress. These strategies allow patients and families to regain a sense of control over their situation, which can alleviate feelings of helplessness. The findings were also supported by the study of (Chambers et al, 2012), who addressed the unmet supportive care needs of psychological distress among cancer patients.
Support mechanisms, such as counselling and support groups, were also shown to have a significant positive impact. Counselling services, in particular, were associated with significant reductions in anxiety and depression, suggesting that professional psychological support is essential in managing the emotional challenges posed by cancer. The findings were supported by the study of Northhouse et al (2010), who emphasise on interventions with family caregivers of cancer patients.
Conclusion
A cancer diagnosis profoundly affects the psychological well-being of both patients and their families. Effective coping strategies, such as active problem-solving and seeking emotional support, are critical in mitigating these effects. Additionally, professional support mechanisms, including counselling and support groups, play an essential role in helping patients and their families navigate the emotional challenges of cancer. These findings suggest the need for comprehensive psychological care in cancer treatment programmes to enhance the emotional well-being of patients and their families.
Nursing Implications
Nurses play a pivotal role in supporting the psychological well-being of cancer patients and their families. As frontline healthcare providers, oncology nurses are uniquely positioned to:
Assess psychological distress regularly using validated screening tools for anxiety and depression.
Provide patient and family education about emotional responses to a cancer diagnosis, normalising these experiences and guiding them toward appropriate support resources.
Encourage active coping strategies, such as problem-solving and seeking social support, by incorporating them into care plans.
Facilitate access to counselling services and support groups, ensuring that patients and families receive timely emotional and psychological support.
Promote holistic care by acknowledging the spiritual and cultural needs of patients and their families, particularly when religious or spiritual practices are used as coping mechanisms.
Recommendations
Counselling services: Healthcare institutions should ensure access to professional psychological services, including individual and family counselling, to provide support throughout the cancer care continuum.
Support group participation: Hospitals and cancer care centres should promote and facilitate patient and caregiver participation in support groups, emphasising the therapeutic benefits of shared experiences.
Training for healthcare providers: Oncology nurses and other healthcare providers should receive regular training in psychosocial care, focusing on the emotional and psychological needs of cancer patients and their families
Research on cultural sensitivity: Future studies should investigate the influence of cultural, spiritual, and religious practices on coping mechanisms among diverse populations to develop more culturally sensitive interventions.
Holistic care models: Cancer care facilities should adopt an integrated approach that combines physical treatment with mental health care, ensuring a comprehensive care model that addresses the psychological impact of cancer on patients and families.
1. Bultz BD, Johansen C. Screening for distress, the 6th vital sign: Where are we, and where are we going? Psycho-Oncology, 2011; 20 (6): 569-71
2. Holland JC, Alici Y. Management of distress in cancer patients. Journal of Supportive Oncology, 2010; 8 (1): 4-12
3. Zebrack B, Kayser K, Sundstrom L, Padgett L, Sundstrom L, Jobin C, et al. A practice-based evaluation of distress screening protocol adherence and medical service utilisation. Journal of the National Comprehensive Cancer Network 2017 Jul; 15 (7): 903-12
4. Jacobsen PB, Donovan KA, Trask PC, Fleishman SB, et al. Screening for psychologic distress in ambulatory cancer patients. Cancer 2005; 103(7): 1494-1502
5. National Comprehensive Cancer Network (NCCN) (n.d.). Practice Guidelines in Oncology. NCCN Guidelines. Retrieved from https:// www.nccn.org
6. Mitchell AJ, Ferguson DW, Gill J, Paul J, Symonds P. Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: A systematic review and meta-analysis. The Lancet Oncology 2013 Jul; 14 (8): 721-32
7. Linden W, Vodermaier A, Mackenzie R, Greig D. Anxiety and depression after cancer diagnosis: Prevalence rates by cancer type, gender, and age. Journal of Affective Disorders 2012 Dec; 141 (2- 3): 343-51
8. Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW. Interventions with family caregivers of cancer patients: Meta-analysis of randomized trials. CA: A Cancer Journal for Clinicians 2010 SepOct; 60 (5): 317-39
9. Chambers SK, Morris BA, Clutton S, Hutchison S, Turner J, Morris B, et al. Psychological distress and unmet supportive care needs in cancer patients and carers who contact cancer helplines. European Journal of Cancer Care 2012 Mar; 21 (2): 213-23
10. Normen M, Agarwal A, Mishra S, Vidhubala E, Shewade HD, Kathiresan J, et al. Patients with cancer are distressed! Indian healthcare provider perspectives on distress screening and referrals to psycho-oncology services - A mixed methods study. Indian Journal of Palliative Care 2021 Oct-Dec; 27 (4): 561-70

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.