Dementia is a condition of the brain disease, usually of a chronic or progressive nature. In person with dementia there is disturbance of multiple higher cortical functions, including memory. The term ‘dementia’ was first coined by Sidney Katz in 1950. The most prominent highlight of the Dementia India Report 2010 was that over 3.7 million Indian people with dementia are cared for by their family members. In India, among Indian adults over 60 years old an estimated 8.8 m million (7.4%) live with dementia (Lee et al, 2023).
Family caregivers of people with dementia, often called the invisible second patients, have a critical role in improving the quality of life of the care recipients. The effects of being a family caregiver, though sometimes positive, are generally negative, with high rates of burden and psychological morbidity as well as social isolation, physical ill-health, and financial hardship. Caregivers vulnerable to adverse effects can be identified, as can factors which ameliorate or exacerbate burden and strain. Indian literature shows that most caregivers of dementia patients experience significant burden and strain (Srivastava et al, 2016; Prince, 2009). Factors contributing to the burden can be studied and efforts can be made to address them so as to reduce caregiver burden, but there are few studies done in the urban Indian population on this subject.
As the health care services continue to improve worldwide, the ageing of the population becomes a natural consequence and brings with it all the problems and diseases associated with ageing. In the coming decades, the major public health problems are likely to be those involving the geriatric population, with dementia being one of the most significant. This is an enormous cause for concern because dependence on others is a crucial factor that separates dementia from other disorders. Therefore, assessing and analysing the problems faced by the caregivers becomes an integral part of the management of dementia. Most of the data in this regard comes from the western world, whereas it is known that most patients of dementia in low- and middle-income countries are managed at home by their family members. And yet there continues to be a paucity of information from such regions, resulting in a gap in the literature. Studying these issues in developing countries will throw light on the problems faced by the caregivers, which will eventually help to create strategies to manage these problems effectively (Srivastava et al, 2016; Mansfield et al, 2022).
Review of Literature
The review of literature was carried out on the PubMed database using the keywords ‘dementia’, ‘caregiver burden, ‘activities of daily living’, and ‘behavioural disturbances’.
The term ‘activities of daily living (ADLS)’ is to collectively describe fundamental skills required to independently care for oneself, such as moving or ambulating, feeding, dressing, personal hygiene, continence and toileting (Edenmekong et al, 2023). ADLS are indicative of the patient’s overall functioning. A decline in the ability to perform ADLS is a characteristic feature of dementia. The ADLS begin to decline more rapidly in the transition from mild to moderate to severe dementia. When the patient is no longer able to perform the basic activities of daily living, the condition can lead to unsafe or unsanitary living conditions and reduce the overall quality of life. Further, it may make the person gradually dependent on other human beings, thereby greatly affecting the cost of care. In higher-income countries, mechanical devices may assist the patient, but these facilities may not be available in developing countries. Nurses are often the first to note the decline in the patient’s abilities when hospitalised therefore, nursing assessment of ADLS is almost always recommended and carried out (Edenmekong et al, 2023). In 2011, a survey from the United States indicated that 20.7 percent of people older than 85 and 7 percent of those aged 75 and 84 needed help with their ADLS (Wolff et al, 2016; Adams PF et al, 2012). However, it is not certain whether these statistics can apply to India and the other Asian countries.
Behavioural and Psychological Symptoms of Dementia (BPSD) can be defined as a wide range of non-cognitive symptoms involving perception (hallucinations), mood (depression, anxiety), behaviour (aggression, disinhibition) and personality. Kim et al (2021) showed that more than 50 percent of patients with dementia suffer from at least one BPSD symptom sleep disturbance being the most common followed by irritability and apathy. About 40 percent of these problems are clinically significant. Care giver burden can be defined as the strain or load borne by a person who cares for a chronically ill, disabled or elderly family member (Srivastava et al, 2016).
Feeling burdened or distressed by the demands of caregiving is the most frequently reported outcome of caregiving (Sinha et al, 2017). Studies from across the globe show that the caregiver burden can adversely impact the health of the caregivers and the patient apart from the inability to interact effectively with the healthcare professional during the illness. Lastly, they may experience burnout and unable to perform the caregiving duties, resulting in compromised patient care (Lin et al, 2019). However, once again, given that the family dynamics vary greatly in the Indian subcontinent, more studies from India are needed.
Razani et al (2007) showed that as the ability to perform ADLS independently declines, the caregiver burden increases (Kales 2015; Kales et al, 2015; Sinha et al, 2017). Many studies show that as the prevalence of BPSD symptoms increases, caregiver burden also increases (Kim et al, 2021; Razani et al, 2007). BPSD symptoms are highly distressing because they are unpredictable, disruptive, difficult to manage, potentially embarrassing or abusive and sleep-depriving to both the patient and the caregiver (Cheng, 2017).
Objectives
The current study sought to: (a) explore the burden perceived by the caregivers of dementia patients as diagnosed by ICD 10 criteria (WHO) in terms of their scores on the Care Giver Burden scale (Zarit et al, 1980)
(b) establish the correlation of this burden with the (i) capacity of the patients to carry out activities of daily living measured by the Katz Index of Independence in Activities of Daily Living (Graf, 2021), and (ii) behavioural and psychological symptoms seen in these patients assessed using the Cohen-Mansfield Agitation Inventory (Cohen-Mansfield J,2008).
Ethical consideration:
The approval for the conduct of the study was accorded by the Institutional Ethics Committee of Bhabha Atomic Research Centre Hospital (BARCH). Data were collected from the participants who gave informed consent. All the data were kept confidential.
Materials and Methods
A semi-structured proforma was specially designed to collect the socio-demographic and illness-related variables. The Caregiver Burden scale (Zarit et al, 1980) was used to assess caregiver burden. This scale has 22 items, and it is one of the most widely used scales to assess caregiver burden in nations across the world. A score of 0 to 20 indicates little or no burden, 21 to 40 indicates mild to moderate burden, 41 to 60 indicates moderate to severe burden, and 61 and above indicates severe burden. The Katz Index of Independence in Activities of Daily Living was used to assess the patient’s capacity to perform the basic activities of daily living. This scale assesses the six activities of daily living, viz. bathing, dressing, toileting, transferring, continence, and feeding. A score of 6 indicates high independence, while 0 indicates complete dependence. This instrument has been used for over three decades.in a variety of settings. The Cohen-Mansfield Agitation Inventory Short (Cohen-Mansfield J, 2008) was used to score the level of behavioural and psychological symptoms of dementia in the patients. This scale assesses the physical and verbal aggressive and non-aggressive behaviours of the patient. The scale is worded in simple language so that it can be easily understood. A higher score indicates higher levels of behavioural and psychological symptoms of Dementia.
The study was designed to be a cross-sectional observational to be conducted over six months. The study population consisted of the persons covered by the Contributory Health Care Scheme (CHSS) by the Department of Atomic Energy. The study was conducted in the Outpatient Department of Psychiatry, BARC Hospital, Anushakti Nagar, Mumbai. Patients diagnosed with Dementia as per ICD-10 were first identified. The family members of these patients who were the primary caregivers of the patients were then selected. Caregiver of a patient who had received a diagnosis of Dementia of any type as per International Classification of Diseases-10 (ICD) (WHO) was identified as the person who was living with the patient and was responsible for caring for the patient daily, most of the time, and was included in the study. The caregivers of patients who were hospitalised for any reason were excluded. Informed consent was then taken. The sample size was calculated using the Open Epi software (Dean et al, 2009). During the study period, we expected to see 65 patients suffering from dementia being cared for by their family members. The prevalence of burden in this population was assumed to be 50 percent to get the highest possible sample size. The formula used is: n = [DEFF*Np(1-p)]/ [(d2/Z2 1-α/2*(N-1) +p*(1-p)] (n=120 p=50 d=5).
We got the sample size of 54 with a confidence limit of 5 percent and a confidence level of 95 percent. We rounded it to 55. However, we were able to collect data from 61 patients during the study period. Convenience sampling was used. The caregiver burden in these family members was assessed using the Caregiver Burden scale (Zarit et al, 1980) The patient’s capacity for activities of daily living was assessed using the Katz Index of Independence in Activities of Daily Living (Graf, 2021). The behavioural and psychological symptoms in dementia patients were assessed using the Cohen-Mansfield Agitation Inventory (CMAI) (Cohen-Mansfield, 2008). The data were pooled and statistically analysed using SPSS software (IBM Corp, 2022). The socio-demographic variables of the caregivers have been expressed in terms of frequency and percentages. The scores on the three scales have been expressed in terms of mean and standard deviation. The severity of the burden has been expressed in terms of frequency and percentages. The scores on the scale for burden were correlated with the scores on the activities of daily living scale and the scores for the behavioural and psychological symptoms of dementia using the Spearman correlation coefficient test. Statistical significance was set at p < 0.05
Results
Socio-demographic variables: The age of the caregivers ranged from 30 to 80 years, with a mean age of 54.2 years and a standard deviation + 8.88 years; 29 (47.5%) of the caregivers were male and 32 (52.5%) were female. As for family structure, 18 (29.5%) of the elderly patients with dementia lived only with their spouses, and thus, the family consisted of only the elderly couple living by themselves; 43 (70.5%) lived with other family members, viz., children and grandchildren. Seven (11.5%) husbands were the caregivers of their wives having dementia, whereas the wife was the caregiver in 14 (23%) cases. Sons were caregivers in 7 (11.5%) cases and daughters in 10 (16.4%) cases, daughters-in-law in 5 (8.2%) cases. In 18 (29.5%) cases, multiple caregivers shared the job.
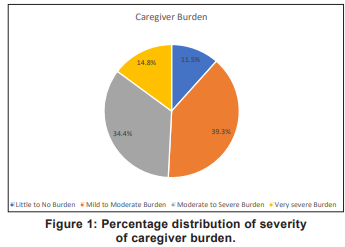
Illness-related variables: 8 (13.1%) patients had a duration of illness up to 2 years, 5 (8.2%) had a duration of 2 to 5 years, and 48 (78.7%) had a duration of illness of more than 5 years. On the Caregiver Burden scale (Zarit et al, 2018), used to assess caregiver burden, the scores ranged from 1 to 76, the mean score being 37.2 + 15.9. Of the caregivers studied, 7 (11.5%) experienced little to no burden, 24 (39.3%) experienced mild to moderate burden, 21 (34.4%) reported moderate to severe burden while 9 (14.8%) were suffering from very severe burden (Fig 1).
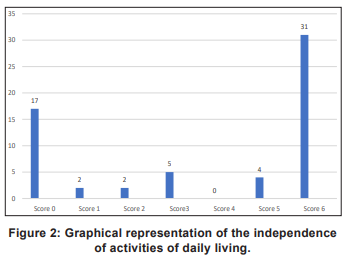
Activities of daily living (ADLS): On the Katz Index of Independence in ADLS (Graf, 2021), the mean score was 3.72 + 2.66, indicating a medium level of dependence of the patient on their caregivers for basic ADLS. 17 (27.9%) scored a zero on this scale, indicating complete dependence on the caregivers (Fig 2).
Behavioural and Psychological Symptoms of Dementia (BPDS): Cohen-Mansfield Agitation Inventory (Cohen-Mansfield,2008) Short was used to evaluate the behavioural and psychological symptoms of dementia exhibited by the patients. The scores ranged from 28 to 110 with a mean of 45.68 + 18.4.
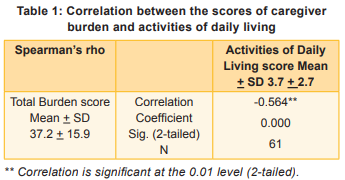
Correlation of caregiver burden with activities of daily living (ADLS): There was a significant negative correlation between the two parameters, indicating that as the scores on the activities of daily living went down, i.e. the patient became more dependent on the caregiver, their burden increased (Table 1).
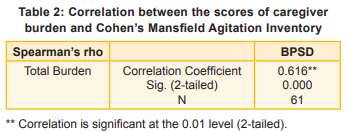
Correlation of caregiver burden with behavioural and psychological symptoms of dementia (BPSD): There was a significant positive correlation between the two parameters, indicating that as patients exhibited more and more behavioural and psychological symptoms, the caregiver burden increased (Table 2).
Discussion
In our study, 49.2 percent of the caregivers experienced moderate to severe burden. This indicates that half the caregivers are significantly burdened by their caregiving chores. Our study concurs with other Indian studies, such as the ones done by Srivastav et al (2016), in which all the caregivers experienced mild to moderate burden. Pattanayak et al (2009) also echoed similar findings. Yet another study from West Bengal (Basu & Mukhopadhyaya, 2022) reported that 60 percent of the caregivers in their sample experienced a severe level of burden.
Our findings are significant because in Indian settings, the care of the dementia patient is usually provided by the family members, and this can continue year after year, with the patient often showing no improvement rather a gradual progression of the disease despite extensive efforts and treatment. Burden is thus the complex reaction to physical, psychological, emotional, social and economic stressors connected with the caregivers’ experience. It has also been reported that caregiver burden among main caregivers is an independent risk factor for higher death rate (Basu & Mukhopadhyaya, 2022).
In our study, as the abilities of the patients to carry out their activities of daily living decreased, the caregivers’ burden also increased. Sinha et al (2017) reported comparable findings. Studies show that caregivers in developing countries spend a median of 3 to 6 hours a day with the person with dementia and 3 to 9 hours assisting with activities of daily living (Dementia Research Group, 2004). As a result, they may face many obstacles as they have to balance caregiving with other demands such as child rearing, career and relationships (Cassie, 2008). They are therefore at increased risk for burden, stress, depression and anxiety. Numerous studies report that caregiving for a person with dementia is more stressful than caring for a person with a physical disability (Ory et al,1999; Mohide EA et al, 1988; Shulz et al, 1990).
In our study, as the severity of the behavioural and psychological symptoms of dementia increased, the caregiver burden also increased. These findings are in keeping with the study done by Shaji et al (2009), which reported similar findings. Kim et al (2021) and others also found that as the prevalence of BPSD symptoms increases, caregiver burden also increases.
Nursing Implication
There are significant activity limitations in dementia patients, especially as the dementia progresses. Nurses can actively render home care services to assist in these activities, thereby helping the patients as well as reducing the caregiver’s burden. As facilitators in caregiver support in in ventilation and experience sharing, they can play a role in manning helplines for those in distress. As the role of non-pharmacological interventions increases, the opportunities to assume a leadership role in this end-of-life caregiving process are enormous for the nurses.
Conclusion
Caregiver burden in dementia is significant as seen with significant positive correlation between the scores on caregiver burden and the CohenMansfield Agitation Inventory. It increases as the limitations in activities of daily living worsen and as the behavioural and psychological symptoms of dementia increase. Hence, caregiver burden should be anticipated when assessing dementia patients with high degree of limitation in the clinics. Similarly, behavioural and psychological symptoms also need to be looked into at each follow-up, and when patients exhibit a higher level of dysfunction in this domain, the caregivers, too, may be interviewed for the burden it causes them. Relief measures for the caregivers, such as assistance or caregiver support groups, could be initiated.
1. International Classification of Diseases (ICD) - 11: Mental and Behavioural Disorders. World Health Organisation, 2024
2. Dementia India Report 2010. Prevalence, Impact, Costs and Services for Dementia. Alzheimer’s Disease International - Global Alzheimer’s disease chapter
3. Srivastava G, Tripathi RK, Tiwari SC, Singh B, Tripathi SM. Caregiver burden and quality of life of key caregivers of patients with dementia. Indian J Psychol Med 2016; 38: 133-36
4. Prince MJ. The 10/66 dementia research group - 10 years on. Indian J Psychiatry 2009; 51: S8-S15
5. Mansfield E, Bryant J, Nair BR, Zucca A, Pulle RC, SansonFisher R. Optimising diagnosis and post-diagnostic support for people living with dementia: geriatricians’ views. BMC Geriatrics 2022; 22 (1): Article No. 143. https://doi.org/10.1186/ s12877-022-02814-0
6. Lee J, Meijer E, Kenneth M, Ganguli M, Ganguli M, Khobragade P, et al. Prevalence of dementia in India: National and state estimates from a nationwide study. Alzheimer’s and Dementia 2023;19 (7): 2898-2912
7. Edenmekong PF, Bomgaars DL, Sukumaran S, Schoo C. Activities of daily living. 2025, In: StatPearls (Internet), StatPearls Publishing: https://www.ncbi.nlm.nih.gov/books/NBK 470404
8. Wolff JL, Feder J, Schulz R. Supporting family caregivers of older Americans. N Engl J Med 2016 Dec 29; 375 (26): 2513-15
9. Adams PF, Kirzinger WK, Martinez ME. Summary Health Statistics for the US Population: National health interview survey 2012. Vital Health Stat 10. 2012 Dec; 255: 1-110
10. Kim B, Noh GO, Kim K. Behavioural and psychological symptoms of dementia and family care giver burden: A path analysis. BMC Geriatrics 2021; 21: Article No. 160
11. Lin CY, Shih Peri-Yu, Ku Li-Jung E. Activities of daily living function and neuropsychiatric symptoms of people with dementia and caregiver burden: The mediating role of caregiving hours. Archives of Gerontology & Geriatrics 2019; 81: 25-30
12. Razani J, Kakos B, Carla OB, Wong JT, Casas R, Lu P, et al. Predicting caregiver burden from daily functional abilities of patients with mild dementia. J Am Geriatr Soc 2007 Sep; 55(9): 1415-20
13. Kales HC. Common sense: Addressed to geriatric psychiatrists on the subject of behavioral and psychological symptoms of dementia. The American Journal of Geriatric Psychiatry 2015; 23(12): 1209-213. https://doi.org/10.1016/j.jagp
14. Kales HC, Gitlin LN, Lyketsos CG. Assessment and management of behavioural and psychological symptoms of dementia. BMJ 2015; 350, h369. https://doi.org/10.1136/bmj. h369
15. Sinha P, Desai NG, Prakash O, Kushwaha S, Tripathi CB. Caregiver burden in Alzheimer-type dementia and psychosis: A comparative study from India. Asian Journal of Psychiatry 2017; 26: 86-91. https://doi.org/https://doi.org/10.1016/j.ajp
16. Cheng ST. Dementia caregiver burden: A research and update and critical analysis. Curr Psychiatry Rep 2017; 19 (9): 64
17. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist 1980; 20: 649-55
18. Graf C. The Lawton Instrumental Activities of Daily Living (IADL) 2021 Scale: Best Practices in Nursing Care to Older Adults, The Hartford Institute for Geriatric Nursing, New York University, College of Nursing. www.hartfordign.org
19. Cohen-Mansfield J. Agitated behaviour in persons with dementia: The relationship between type of behaviour, its frequency, and its disruptiveness. J Psychiatr Res 2008 Nov; 43 (1): 64-69
20. Dean AG, Sullivan KM, Soe MM. OpenEpi: Open-source epidemiologic statistics for public health. Public Health Rep 2009 May-Jun; 124 (3): 471-74
21. IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp
22. Pattanayak RD, Jena R, Tripathi M, Khandelwal SK. Asian Journal of Psychiatry 2010; 3 (3): 112-16
23. Basu I, Mukhopadhyaya S. Neuropsychiatric symptoms of dementia and caregivers’ burden: A study among Indian caregivers. Dement Neuropsychol 2022; 16 (3): 332-40
24. The 10 / 66 Dementia Research Group. Care arrangements for people with dementia in developing countries. Int J Geriatr Psychiatry 2004; 19: 170-77
25. Cassie KM, Sanders S. Familial caregivers of older adults. J Gerontol Soc Work 2008; 293-320
26. Ory MG, Hoffman RR, Yee JL, Tennstedt S, Schulz R. Prevalence and impact of caregiving: A detailed comparison between dementia and non-dementia caregivers. Gerontologist 1999; 39 (2):177-85
27. Mohide EA, Torrance GW, Streiner DL, Pringle DM, Gilbert R. Measuring the well-being of family caregivers using the time trade–off technique. J Clin Epidemiol 1988; 41 (5): 475-82
28. Shulz R, Visintainer P, Williamson GM. Psychiatric and physical morbidity effects of caregiving. J Gerontol 1990; 45 (5): 181-91
29. Shaji KS, George RK, Prince MJ, Jacob KS. Behavioral symptoms and caregiver burden in dementia. Indian J Psychiatry 2009; 51 (1): 45-49

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.