Diabetes Mellitus (DM) is a long-term metabolic disease marked by high blood glucose, which over time can seriously harm the heart, blood vessels, eyes, kidneys, and nerves. The anticipated prevalence of diabetes worldwide in 2019 was 9.3 percent (463 million people); and it is expected to increase to 10.2 percent (578 million) by 2030 and 10.9 percent (700 million) by 2045 (Ahmed et al, 2023). A patient with DM has a high chance of developing a diabetic foot ulcer (DFU). Awareness and attitude toward the prevention of diabetic foot ulcers are necessary for a better quality of life. Educating patients with diabetes about the methods of foot care plays an important role in preventing diabetic foot complications in individuals with DM. Knowledge and awareness of DM and the related risk factors, complications, and management are necessary for better DM control and a higher quality of life (Ahmed et al, 2023).
One effect of diabetes is diabetic foot, which is caused by peripheral artery disease (PAD) and sensory neuropathy in the feet of diabetic patients. The worldwide prevalence of diabetic foot ulcers is reported to be 6.3 percent. It is greater in men (4.5%) and type 2 diabetics (6.4%). This problem is stated to be the commonest cause of hospitalisation for diabetic patients, representing up to 25 percent of all hospital admissions of diabetics. It impairs patients’ quality of life and their psychological and physical performance thus incurring significant costs for health services; their mortality rate is also higher than that of those without a diabetic foot (Al-Hariri et al, 2017). Diabetic foot ulcers are highly complicated, and a serious problem for the community also. Previous reports found that identifying people at high risk and managing the risk factors early can reduce the outcomes of diabetic foot ulcers and lower extremity amputations. The practice of diabetic foot care, including daily foot examination and use of appropriate footwear is important in its early detection and prevention of complications.
Diabetic foot frequently necessitates extended hospitalisation, which raises costs. It is regarded as one of the leading causes of disability and death in diabetics and a major public health issue imposing a significant socio-economic burden. Therefore, policymakers and academic researchers are focusing more on preventive aspects of diabetic foot.
Diabetic footispreventable; early identification can bring down amputation rates by up to 80 percent. People with poor knowledge and practice regarding diabetic foot care are known to have a higher incidence of diabetic foot ulcers. Proper control of blood glucose prevents the development of microvascular complications. Poor foot care knowledge and practices are important risk factors for foot-related problems among diabetic people (Mandal et al, 2023).
National hospital discharge data indicate that the average hospital length of stay in diabetic patients with ulcer diagnoses was 59 percent longer than in those diabetes discharges without them. While 14-20 percent of patients with foot ulcers subsequently require an amputation, foot ulceration is the precursor to approximately 85 percent of lower extremity of amputations in persons with diabetes.
During exposure to various clinical areas, statistical information was collected from a diabetic out-patient department. The values showed that approximately 75 patients are attending diabetic clinic per day and 3,510 patients had attended the clinic during the year 2023-24. The investigator came across several patients getting admitted to the hospital with diabetic foot ulcers. Despite regular medication intake and regular follow-up visits, patients still end up with complications. This scenario inspired the investigators to assess the level of risk for the development of diabetic foot ulcer.
Need for the study:
A few studies have been conducted to assess the level of awareness and knowledge among diabetic patients. Hence this study was undertaken to evaluate the risk factors for diabetic foot ulcers to improve foot care practice among diabetes patients.
Objectives
The study was carried out to (a) assess the level of knowledge and practice on diabetic foot ulcer among patients with diabetes mellitus; (b) identify the risk factors for the development of diabetic foot ulcer; (c) correlate total risk and its components regarding diabetic foot ulcer; and (d) associate the level of risk factors for developing foot ulcer with selected demographic and clinical variables.
Review of Literature
Satabdi et al (2023) conducted a cross-sectional study over three months among 310 diabetic outpatients of a medical college in an eastern Indian state. Data were collected with a validated questionnaire containing socio-demographics, clinical and behavioural factors, foot care knowledge and practice and the SINBAD score was used for assessing diabetic ulcers. Out of 310 participants, 44 (14.2%) had diabetic foot ulcer, and one-fifth of them had a SINBAD score ≥3, indicating severity. Knowledge level was poor among 245 (79.0%), and healthy foot habits were among only 70 (22.6%). Addiction, diabetes for ≥5 years, any associated non-communicable diseases, irregular treatment and follow-up care, unhealthy foot condition, improper footwear, poor knowledge of the disease and unhealthy foot habits had a significant association with the occurrence of foot ulcers.
Lawrence ST et al conducted a study on the knowledge and practice of diabetic foot care and the prevalence of diabetic foot ulcers among diabetic patients of selected hospitals in the Volta Region, Ghana. A multihospital-based cross-sectional study was conducted among 473 patients with DM who were recruited using the systematic sampling method. Data were collected using a validated, pre-tested, and structured questionnaire, while medical variables were obtained from patient folders and analysed using SPSS version 23. The results showed that 63 percent of diabetic patients had good knowledge of DFU, while 49 percent competently practised it. The prevalence of DFU was 8.7 percent among the studied diabetic patients. Male diabetic patients were 3.4 times more likely to develop DFU than female diabetic patients. The study found that there was good knowledge but poor practices of DFU among patients. Health care providers are expected to better educate patients and emphasise self-care practices to patients. Health care providers should also give more attention to patients with associated risk factors to avoid further complications and reduce the occurrence of DFU.
Chin-Siang et al (2024) conducted a crosssectional design and collected data through selfreported questionnaires administered to a sample of 586 patients from five medical centres. The descriptive and inferential analyses were used to explore the relationships between potential risk and protective factors and foot care behaviours. Overall, 429 individuals (73.2%) had good foot care behaviours, while 157 (26.8%) displayed poor foot care behaviours. Furthermore, the study identified eight influencing factors on foot care behaviours, including smoking status, the availability of a caregiver, the presence of diabetic foot ulcers, amputation history, and foot care knowledge, subjective norms in diabetes self-care behaviour, diabetes-related stress, and quality of life index values. The logistic regression analysis showed that current smokers were 60 percent less likely to practice good foot care compared to non-smokers (odds ratio [OR] = 0.40; 95% confidence interval [CI] = 0.22–0.73). Having a caregiver decreased the likelihood of practicing good foot care by 50 percent (OR=0.52; 95% CI = 0.33–0.84), while having diabetic foot ulcers doubled it (OR=2.65; 95% CI=1.26–5.54). Additionally, more foot care knowledge increased the likelihood by 20 percent (OR=1.21; 95% CI=1.10–1.33), and higher diabetes-related stress increased it by 1.03 times (OR=1.03; 95% CI=1.02–1.05).
Alrashed et al (2024) conducted a crosssectional study to investigate the impact of the education levels of diabetic patients on diabetic foot care knowledge and practice. A convenient sampling technique was conducted on 534 patients with diabetes mellitus from public and private care hospitals. The data was collected using a validated, pre-tested and structured bilingual (Arabic, English) questionnaire. There were 534 patients interviewed, 39.1 percent of whom were males and 60.9 percent females; 61.4 percent of the patients had T2DM for over 10 years. There was a significant difference in education levels between the male and female patients (53.8% and 46.2%, p = 0.001). Furthermore, 83.9 percent patients were married. The difference in education between the married and the single, divorced, and widowed patients was significant (p = 0.007). Patients with uncontrolled HbA1c were 2.43 times more likely to have hypertension (RR = 2.43, p = 0.03), while patients with highly uncontrolled diabetes had 3.1 times more chances of hypertension (RR = 3.1, p = 0.009). Heart disease prevalence was 3.27 times higher in diabetes patients with uncontrolled HbA1c and 3.37 times higher in patients with highly uncontrolled HbA1c. Patients with diabetes who have been diabetic for more than 10 years have a greater risk of heart disease (RR = 2.1; p = 0.03). Patients with lower education levels exhibited more diabetic complications compared to patients with higher education levels (p < 0.05). The present study highlights the importance of education and awareness campaigns targeting diabetic patients, especially those with lower education levels, to improve diabetes control and prevent, or manage, comorbidities. Healthcare providers should also prioritise patient education and medication adherence to improve diabetes management and reduce the risk of complications.
Methodology
The research design adopted for the study was descriptive type. Its setting was, Kovai Medical Centre & Hospital (KMCH), Coimbatore. The study population consisted of DM patients attending the outpatient department of KMCH.
Inclusion & exclusion criteria:
Patients diagnosed to have type 2 diabetes mellitus; both male and female patients between the age of 30-80 years; patients who were able to speak Tamil or English; patients with co-morbid diseases like hypertension/kidney, and cardiac & peripheral vascular diseases were included. Patients who have already developed diabetic foot ulcer were excluded.
Data collection tool:
The time period for data collection was one week. The investigator collected the data from 5-7 subjects every day and time taken for each subject was 10-15 minutes; 60 participants were involved in this study. Diabetes foot care questionnaire was used to assess the patient’s Self Care Practices in the prevention of diabetic foot ulcer. The investigator also used the Diabetes Foot Risk Assessment Form Guide and the Diabetic Foot Risk Assessment Tool-Diabetes Care Program of Nova, Scotia September 2009 to identify the level of risk for developing diabetic foot ulcer among patients with type 2 diabetes mellitus.
Out of the 60 subjects, 51 (85%) had moderate risk and 9 (15%) had high risk and the item total correlation values are significant at 0.1 levels. which reveals that the most predominant risk factor is vascular changes. The second predominant risk factor was limitation of mobility whereas the last risk factor was foot wear practices
Data analysis:
Descriptive and inferential statistics was used to analyse the data.
Results
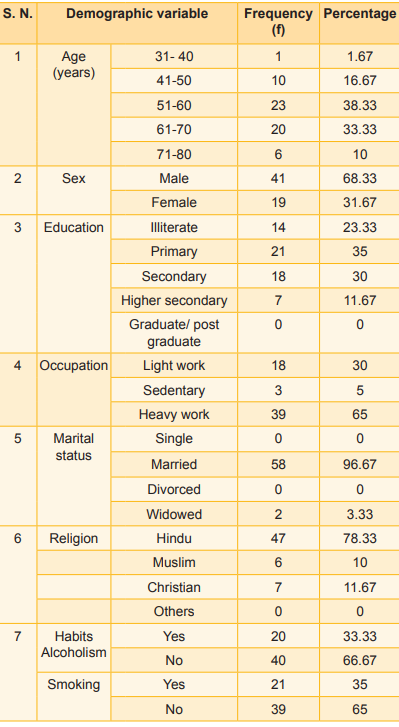
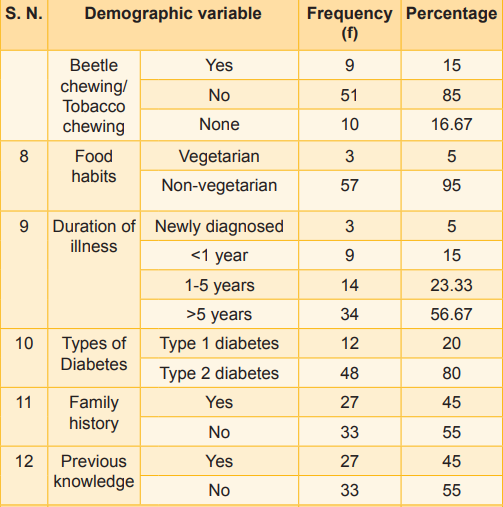
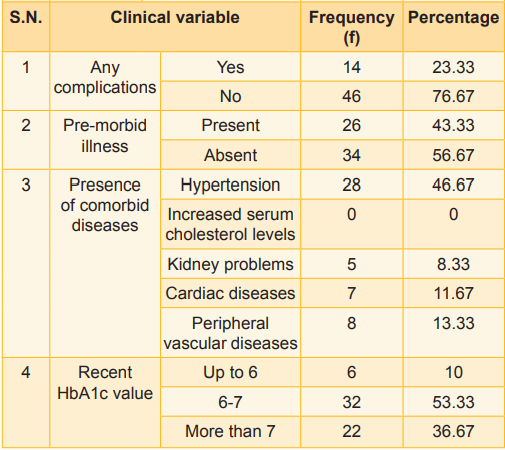
It was seen that 41 (68.33%) were males and 19 (31.67 %) females. There was one subject (1.66%) aged 31-40 years, 10 (16.67%) were in 41-50 years range, 23 (38.33%) between 51-60 years, 20 (33.33%) between 61-70 years, and 6 (10%) 71-80 years of age; 14 (23.33%) were illiterate, 21 (35%) had primary education, 18 (30%) secondary education, 7 (11.67%) higher secondary education and none with graduation/post-graduation status. Occupation: 18 (30%) were light workers, 3 (5%) sedentary workers and 39 (65%) heavy workers. Marital status: none were single, 58 (96.67%) were married; none were divorced and 2 (3.33%) were widowed (Table 1). Religion: 47 (78.33%) were Hindu, 6 (10%) Muslim and 7 (11.67%) were Christian. Habits: 20 (33.33%) consume alcohol and 40 (66.67%) do not consume alcohol; 21(35%) were smokers and 39 (65%) were non-smokers; 9 (15%) were beetle/tobacco chewers 51 (85%) had no habit of beetle/tobacco chewing. Food habits: 3 (5%) were vegetarians and 57 (95%) non-vegetarian.
Table 1: Description of demographic and clinical variable of patients (N=60)
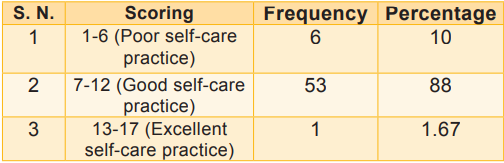
It was seen that out of 60 samples, 2 (3%) had poor knowledge, 15 (25%) had moderate knowledge, and 43 (72%) had good knowledge (Table 2). Table 3 shows that out of 60 samples, 6 (10%) had poor self-care practice, 58 (88%) had good self-care practice, and 1 (1.6%) had excellent self-care practice.
Table 2: Distribution according to level of knowledge about diabetic foot ulcer (N=60)
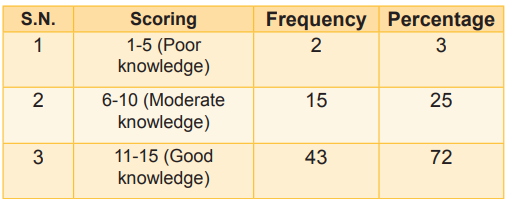
Table 3: Distribution according to the prevention practice assessment of DM patients (N=60)
It was seen that out of 60 samples, 51 (85%) had moderate risk for development of diabetic foot ulcer whereas 9 (15%) had high risk for development diabetic foot ulcer (Table 4).
Table 5 depicts the rank correlation between total risk and its factors for developing diabetic foot ulcer. Correlation value of limitation of mobility was 0.0445, vascular changes was 0.060, sensation of feet was 0.050, skin conditions was 0.034, structural deformities was 0.025, diabetic neuropathy was 0.055, and footwear practices were 0.0001. The item total correlation is significant at the 0.01 level, and it was revealed that the most predominant risk factor was vascular changes, the second predominant factor was sensation of feet, whereas the last risk factor was footwear practices. In Table 6, the ?2 (15.953) was significant showing that there was an association between age and the level of risk for the development of diabetic foot ulcer.
Table 4: Distribution of patients according to the risk of development of diabetic foot ulcer (N=60)
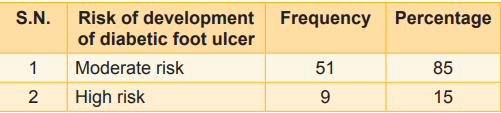
Table 5: Correlation between total risk and its components regarding diabetic foot ulcer
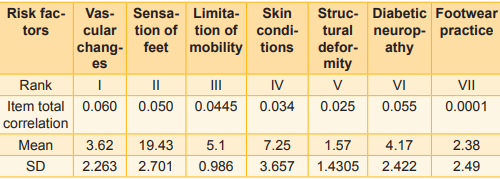
Table 6: Association between age and the level of risk for the development of diabetic foot ulcer
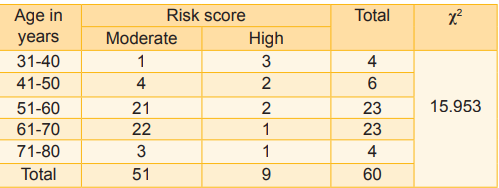
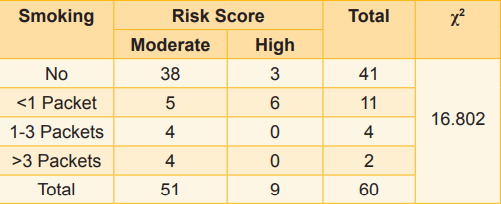
Table 7: Association between smoking habits and the level of risk for the development of diabetic foot ulcer
p<0.05
Table 7, ?2 value as 16.802 was significant showing that there was an association between smoking habits and the level of risk for the development of diabetic foot ulcer.
Discussion
The present study was designed to assess the level of risk for developing diabetic foot ulcer, and a descriptive study design was adopted.
The mean age of the study participants was found to be similar to a study by Pavithra et al (2020) where the average age was 56.98 (10.54). However, in another study (2019–20), the average age was found to be lower than in our study (49.37 ± 1.16). Similar to a study in Tamil Nadu, in our study male participants were more (68.33%) than females (31.67%). However, in other studies, females’ diabetes rates are higher than males.
Similar to a study in Haryana (India) by Verma et al (2012), around half of our study participants had a family history of diabetes (45%). In the present study, almost three-fourths of the diabetics are taking treatment for a comorbidity or a chronic disease; 43.33 percent participants had health problems other than diabetes (Deribe et al, 2014). Hypertension was the most common comorbidity in our study. In a multicentre study in India, hypertension among diabetics was found to be 34 percent (Viswanathan et al, 2005).
In the present study, more than half of the diabetic patients had a good knowledge score, which is similar to other studies (Deribe et al, 2014; Pourkazemi et al, 2020). Imparting knowledge at the primary care level will bring behavioural change and improve the practices. The knowledge score in the present study is higher than the scores reported in other studies (Singh et al, 2020; Dixit et al, 2011). In another study Singh et al (2020) concluded that there was a lack of awareness about diabetes and its complications, and they recommended creating awareness of diabetic foot.
Half of our study participants were inspecting their feet daily. In a multicentre study, it was found that 71.4 percent of urban and 76 percent of rural populations inspected their feet daily and 54 percent wore footwear all the time. In another multicentre study in India, it was found that 65 percent of type 2 diabetics do not follow foot care practices, and 90 percent wore footwear outdoors, and 3 percent wore footwear indoors. Barefoot walking is practised by 7 percent of the study subjects (Olowo et al, 2020). In our study, around 10 percent of diabetics wear footwear indoors. In general, wearing footwear indoors is not practised here. Diabetic patients who walk barefoot for any reason may be advised on the importance of footwear. Less than half of the participants dry their feet between the toes after washing and inspect their footwear before wearing it (Taksande et al, 2017). Educating diabetic patients on foot care practices and the right methods of use of footwear will help the patients to prevent calluses and foot ulcers.
In our study, good knowledge and regular physical activity are positively associated with good foot self-care practices. Higher education, higher physical activity, and a previous history of diabetic foot ulcers were found to be significant predictors of good foot care practices (Pourkazemi et al, 2020). In another study, good practice score was found among secondary schooling and patients on insulin (Dixit et al, 2011). Less education, poor socioeconomic status, and unawareness of foot care were contributing to improper footwear practices (Taksande et al, 2017).
In our study, more than half of the participants had at least one of the clinical findings related to diabetic foot. At the primary care level, checking for the presence of peripheral neuropathy and foot examination may be given special importance. This will help in the prevention of diabetic foot. There is a definite need to improve the knowledge of diabetic patients regarding foot care practices. Hence, every follow-up visit at the primary care level may be utilised for reinforcing the foot care practices.
The rank correlation between total risk and its factors for developing diabetic foot ulcer. Correlation value of limitation of mobility was 0.0445, vascular changes 0.060, sensation of feet 0.050, skin conditions 0.034, structural deformities 0.025, diabetic neuropathy 0.055, and footwear practices were 0.0001. The item total correlation is significant at the 0.01 level, which reveals that the most predominant risk factor was vascular changes, followed by sensation of feet, whereas the last risk factor was footwear practices.
The findings of the study indicated that there was a significant association between the demographic profile, like age and smoking, with the level of risk for developing diabetic foot ulcer, significant at p< 0.01 and p<0.05. This shows that there was an association between the demographic variables and total risk score.
Recommendations
A similar study can be conducted between rural and urban diabetic patients; a study can be replicated in different settings; a study can be conducted with a large sample in a community set-up to improve the knowledge of the clients, another study can be conducted as an interventional study.
Conclusion
In this study, 51 (85%) patients had moderate level risk and 9 (15%) had high risk; the most predominant risk factor was vascular changes; the second predominant risk factor was sensation of feet, whereas the last risk factor was footwear practices. There was a relationship between age and smoking with the total risk of developing foot ulcers and no relationship between sex, co-morbid illness, duration of illness and HbA1c with total risk for developing foot ulcer. Vascular changes and sensation of the feet play an important role in developing diabetic foot ulcers.
1. Metwally Ahmed, Aljohani ZA, Maashi MI, Alrehaili AA, Alrehaili BM. Aljabri AM, et al. Knowledge, attitude, and practice regarding the risk of diabetic feet among diabetic patients in the Madinah Region, Saudi Arabia. Cureus Apr 2023; 15 (12): e49933. DOI 10.7759/cureus.49933. Available from https://pubmed.ncbi.nlm.nih.gov/38058528/
2. Al-Hariri MT, Alenazi AS, Alshammari DM, Bahamdan Ahmed, Al-Khtani SM, Abdulwahab AA, et al. Descriptive study on the knowledge, attitudes and practices regarding the diabetic foot. Journal of Taibah University Medical Sciences 2017 Dec; 12 (6): 492-96. Available from https://doi.org/10.1016/j. jtumed.2017.02.001
3. Huimin Jia, Xiaocheng Wang, Jingmin Cheng. Knowledge, attitudes, and practices associated with diabetic foot prevention among rural adults with diabetes in North China. Frontiers in Public Health. May 2022; 20: 10.876105. doi: 10.3389/fpubh.2022.876105). Available from - https:// pmc.ncbi.nlm.nih.gov/articles/PMC9163951/pdf/fpubh10-876105.pdf
4. Mandal Amit, Thomas Nihal, Zachariah Anand, Mathuram AJ. Diabetic Foot Care: Knowledge and Practice – A Cross-sectional Study from a Tertiary Care Hospital in Southern India. Matrix Science Medica, published by Wolters Kluwer - Medknow 2023 Aug 7: 76-81. https:// www.cmcendovellore.org/wp-content/uploads/Diabetic-Foot-Care-Knowledge-and-Practice.pdf
5. Mitra Satabdi, Majumdar KK, Sushanta Bhanja. Prevalence of diabetic foot ulcers and assessment of foot care knowledge and practice among patients attending the diabetic clinic of a tertiary hospital of eastern India. International Journal of Community Medicine & Public Health 2023 Jul; 10 (7): 2500-05. Available from - https://www. ijcmph.com/index.php/ijcmph/article/view/11228
6. Tuglo LS, Nyande FK, Agordoh PD, Nartey EB, Pan Z, Logosu L, et al. Knowledge and practice of diabetic foot care and the prevalence of diabetic foot ulcers among diabetic patients of selected hospitals in the Volta Region, Ghana. International Wound Journal 2022; 19: 601-14. Available form -https://pubmed.ncbi.nlm.nih. gov/34190402/
7. Chin-Siang Ang, Goh KFI, Lodh Nandika, Qin VM, Liew Huiling, Sidhu HRS, et al. Foot care behaviours and associated factors among patients with type 2 diabetes: A cross-sectional study. Journal of Global Health 2024; 14. 04145. doi: 10.7189/jogh.14.04145). Available from https://pubmed.ncbi.nlm.nih.gov/39173154/
8. Alrashed FA, Iqbal Muhammad, Al-Regaiey KA, Ansari AA, Asma AA, Alderaa AA, Alhammad SA, et al. Evaluating diabetic foot care knowledge and practices at the education level. Medicine 2024; 103 (34): e39449. doi: 10.1097/MD.0000000000039449.) Available from https:// pubmed.ncbi.nlm.nih.gov/39183414/
9. Pavithra H, Akshaya KM, Nirgude AS, Balakrishna AG. Factors associated with awareness and practice about foot care among patients admitted with diabetes mellitus: A cross-sectional research from a medical college hospital of southern India. Nepal J Epidemiol 2020; 10: 897904 https://pmc.ncbi.nlm.nih.gov/articles/PMC7538014/
10. Shamim M, Alhakbani MS, Alqahtani MS, Alharthi OS, Alhaqbani YJ. Knowledge, attitude, and practice regarding diabetic foot care among Saudi and non-Saudi diabetic patients in Alkharj. J Family Med Prim Care 2021; 10:85964. Available from - https://pubmed.ncbi.nlm.nih. gov/34041089/
11. Verma M, Sharma N, Rashi VA, Bashar MA, Nath B, Kalra S. Diabetic foot care knowledge and practices in rural North India: Insights for preventive podiatry. J Association of Physicians of India 2021; 69: 2226. Available from - https://pubmed.ncbi.nlm.nih.gov/33527808/
12. Deribe B, Woldemichael K, Nemera G. Prevalence and factors influencing diabetic foot ulcer among diabetic patients attending Arbaminch Hospital, South Ethiopia. J Diabetes Metab 2014; 5: 17 https://www. iomcworld.com/open-access/prevalence-and-factors-influencing-diabetic-foot-ulcer-among-diabetic-patients-2155-6156.1000322.pdf
13. Viswanathan V, Thomas N, Tandon N, Asirvatham A, Rajasekar S, Ramachandran A, et al. Profile of diabetic foot complications and its associated complications: A multicentric study from India. J Assoc Physicians India 2005; 53:93336. https://pubmed.ncbi.nlm.nih.gov/16515230/
14. Pourkazemi A, Ghanbari A, Khojamli M, Balo H, Hemmati H, Jafaryparvar Z, et al. Diabetic foot care: Knowledge and practice. BMC Endocr Disord 2020; 20 (1): 40 https:// pubmed.ncbi.nlm.nih.gov/32192488/
15. Singh S, Jajoo S, Shukla S, Acharya S. Educating patients of diabetes mellitus for diabetic foot care. J Family Med Prim Care 2020; 9: 36773. https://pubmed.ncbi.nlm. nih.gov/32110620/
16. Dixit S, Maiya A, Khetrapal H, Agrawal B, Vidyasagar S, Umakanth S. A questionnaire-based survey on awareness of diabetic foot care in the Indian population with diabetes: A cross-sectional multicentre study. Indian J Med Sci 2011 Oct; 65 (10): 411-23. https://pubmed.ncbi. nlm.nih.gov/23511041/
17. Olowo S, Iramiot JS, Ssenyonga LV. Knowledge of diabetic foot complication, selfcare beliefs and practices among patients attending a tertiary hospital in Eastern Uganda. Int J Afr Nurs Sci 2022; 16:100402. https://www.sciencedirect.com/science/article/pii/S2214139122000099
18. Taksande BA, Thote M, Jajoo UN. Knowledge, attitude, and practice of foot care in patients with diabetes at central rural India. J Family Med Prim Care 2017; 6: 28487. https://pubmed.ncbi.nlm.nih.gov/29302533/

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.