Medical adhesive-related skin injuries (MARSI) are a significant concern in clinical settings affecting patient safety, comfort, and healthcare outcomes. These injuries, which arise due to improper adhesive use or removal techniques, can lead to extended hospital stays, delayed recoveries, and increased healthcare costs. Although advancements in adhesive technology exist, MARSI remains a prevalent issue in many healthcare institutions globally. Recent global updates emphasise the urgent need for effective strategies to mitigate these injuries and enhance overall patient safety (Kotter et al, 2021; ).
At Rajagiri Hospital, the incidence of MARSI was recorded at 0.33 per 1000 patient days, which prompted the initiation of a comprehensive Quality Improvement Project (QIP) aimed at addressing this issue. This initiative focuses on integrating the latest insights and practices aimed at reducing MARSI, ultimately improving patient outcomes and maintaining high standards of care.
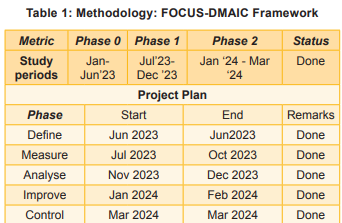
The FOCUS-DMAIC framework, an evidencebased approach used in quality improvement, was applied to systematically address the problem of MARSI. The phases of this framework—Define, Measure, Analyse, Improve, and Control—were followed to create a structured approach to reduce MARSI incidence, improve staff knowledge, and standardise adhesive practices. This study aims to demonstrate the effectiveness of these interventions in reducing MARSI rates and improving patient care quality.
The MARSI incidence of 0.33 per 1000 patient days in Rajagiri Hospital was primarily attributed to suboptimal adhesive materials, improper application and removal techniques, and inadequate staff knowledge. Additionally, there were significant gaps in the knowledge and training of healthcare professionals regarding proper adhesive use. These factors point to the need for targetted interventions to enhance adhesive practices, improve staff knowledge, and reduce MARSI-related injuries.
Objectives
The project set forth the following aims and objectives:
1. Increase healthcare professionals’ adherence to proper adhesive application and removal techniques by 30 percent within six months.
2. Standardise adhesive use protocols across various healthcare settings, achieving 40 percent compliance within six months.
3. Reduce the incidence of MARSI by 25 percent within 12 months.
Need of the Study
This study addresses the critical need to improve the management of MARSI, which not only affects patient comfort but also has implications for healthcare costs and recovery times. By enhancing adhesive practices and training healthcare professionals, this initiative aims to create a safer clinical environment and improve patient outcomes.
Review of Literature
Studies show that proper education and the use of specialised personnel can substantially reduce MARSI rates (Drosdowsky et al, 2020; Earle et al, 2022). Kottner et al (2021) emphasised the role of standardised protocols in reducing MARSI. Jones et al while (2023) found that specialised wound care expertise could significantly lower the incidence of these injuries. Furthermore, the adoption of new adhesive materials, as seen in the work of Drosdowsky et al (2020), plays a crucial role in minimising skin damage.
Several factors contribute to MARSI, including improper adhesive selection, prolonged use, and incorrect application or removal techniques. Drosdowsky et al (2020) found that adhesives like Tegaderm and Dynaplaster were often linked to higher injury rates, especially in high-moisture areas or around medical devices. Patients with comorbidities such as diabetes or immobility are also at greater risk due to more fragile skin.
Training healthcare staff on proper adhesive use is crucial for reducing MARSI. Earle et al. (2022) reported that structured training significantly increased healthcare professionals’ knowledge and reduced MARSI by 30-40 percent. Regular education helps maintain best practices, especially with new adhesive products.
Methodology
Project design: The QIP utilised the FOCUS-DMAIC framework to systematically address the issue of MARSI. This structured approach facilitated clear identification of objectives, measurement of baseline data, and implementation of targetted interventions. The timeline of DMAIC is shown in Table 1.
1. Define: The project team defined the scope and objectives, emphasising the importance of reducing MARSI incidence and improving staff knowledge.
2. Measure: Baseline data was collected to evaluate the current incidence of MARSI and the knowledge level of healthcare professionals regarding adhesive use.
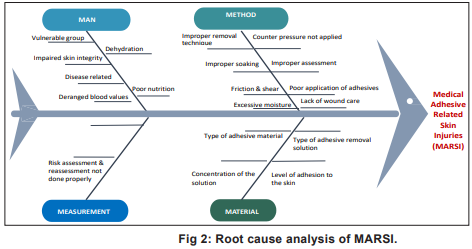
3. Analyse: A root cause analysis was conducted to identify factors contributing to MARSI incidents. This involved assessing materials used, application techniques, and knowledge gaps among staff.
4. Improve: Targetted interventions were implemented based on the analysis to enhance practices and reduce MARSI incidence.
5. Control: Monitoring and feedback mechanisms were established to ensure the sustainability of improvements.
Measurement and Analysis
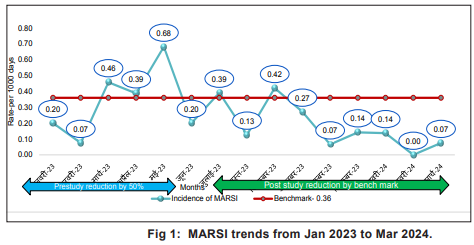
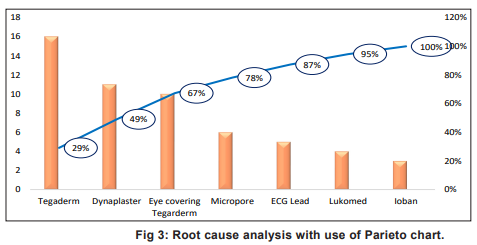
The project focused on specific areas within the hospital, including operation theatre, intensive care units, inpatient wards incidence rates of MARSI to assess the knowledge levels regarding adhesive use among nursing staff and the compliance with updated adhesive usage protocols. The trends and root cause analysis of MARSI are depicted in Figure 1-3.
A thorough root cause analysis was performed using a Fish bone analysis & Pareto chart to identify the most significant contributors to MARSI. Findings revealed that 80 percent cause of MARSI are due to:
• Tegaderm (CVC site and Cannula site)
• Dynaplaster dressing
• Eye covering Tegaderm in OT
• Micropore
A Fishbone diagram and Pareto chart (Fig 3) were used to analyse the root causes of MARSI. Key factors contributing to MARSI included:
Interventions
A series of strategic interventions were implemented to address the identified issues:
1. Formation of wound care champions: Selected staff were designated as wound care champions to promote best practices and serve as resources for their peers.
2. Specialised nurses: Tissue Viability Nurses and Stoma Care Nurses provided expert oversight and support wound care practices and provide expert guidance on adhesive use
3. Introduction of tissue viability nurse & stoma care nurse: A specialised nurse was introduced to oversee wound care practices and provide expert guidance on adhesive use.
4. Policy revisions: Existing protocols were reviewed and updated to reflect the latest evidence-based practices regarding adhesive application and removal.
5. New product implementation: Several new products were introduced, including:
6. Training programmes: Comprehensive training sessions were conducted on adhesive removal techniques, emphasising proper soaking and counter traction to minimise skin injuries.
7. Regular audits: Random audits were conducted for skin assessments to monitor compliance with best practices and identify areas for further improvement.
Results
Pre-QIP Metrics (Jan-Jun 2023)
Before the implementation of the QIP, baseline metrics were established:
• Incidence rate of MARSI: 0.33 per 1000 patient days.
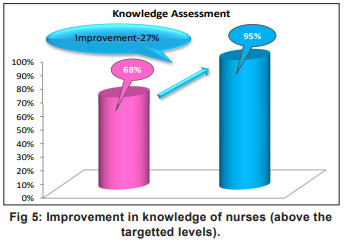
Knowledge of nurses regarding adhesive use: 68 percent.
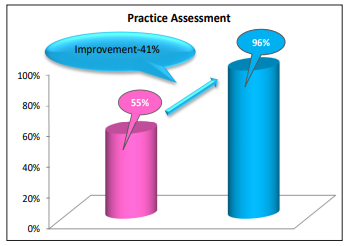
• Accurate usage of adhesives: 55 percent.
Post-QIP Metrics (Jan-Mar 2024)
After implementing the QIP, follow-up metrics were collected:
These results demonstrated a substantial reduction in MARSI incidence, with improvements in nurse knowledge and adhesive usage compliance (Fig 4-6). The reduction in MARSI by 45 percent exceeded the targetted 25 percent, and adherence to correct adhesive practices improved significantly, underscoring the effectiveness of the interventions.
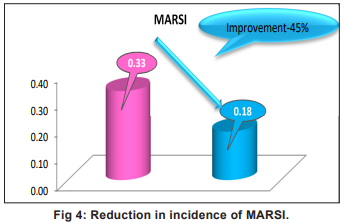
Outcome Analysis
The results demonstrated significant improvements. The incidence rate of MARSI decreased by 45 percent, exceeding the target reduction of 25 percent within 12 months.Nurse knowledge improved by 27 percent, surpassing the target increase of 30 percent within six months. Accurate usage of adhesives rose by 41 percent, significantly above the targetted improvement.
Discussion
The results of this QIP align with findings from previous studies, which suggest that focussed training and protocol standardisation can significantly reduce MARSI rates: (1) The 45 percent reduction in MARSI incidents surpasses the project’s target of 25 percent, demonstrating the efficacy of the interventions. The introduction of specialised staff, such as Wound Care Champions and the Tissue Viability Nurse, was instrumental in providing ongoing support and guidance, aligning with Drosdowsky et al (2020) (2) was appreciated the importance of specialised personnel in reducing MARSI. Furthermore, the incorporation of new products designed to minimise skin injuries directly contributed to the project’s success, echoing findings of Jones et al (2023) that innovative products can significantly impact MARSI rates.
Additionally, the improvement in nursing knowledge from 68 percent to 95 percent highlights the success of the targetted training programmes. These findings support the work of Earle et (2022), who reported that structured education can lead to a significant increase in healthcare professionals’ knowledge and practice.
The positive outcomes of this QIP not only support the findings of similar studies but also emphasise the need for ongoing training, adherence to updated practices, and systematic monitoring to further mitigate MARSI and enhance patient care.
Recommendations
Sustained training programmes: Continuous education on adhesive practices should be institutionalised to keep staff updated on best practices and new products.
Regular audits and feedback: Ongoing audits and feedback sessions should be scheduled to ensure adherence to protocols and identify areas for improvement.
Collaboration with product manufacturers: Engage with manufacturers to explore new adhesive technologies and materials that can further reduce MARSI occurrences.
Nursing Implications
Improve patient safety: Reducing MARSI risk through better adhesive practices enhances overall patient safety.
Ongoing education: Continuous training for nurses is essential to keep them updated on best practices for adhesive use.
Leadership roles: Nurses should take on leadership roles, such as Wound Care Champions, to promote best practices.
Standardised protocols: Implementing and adhering to standardised adhesive protocols ensures consistent patient care.
Regular monitoring: Conducting audits and feedback sessions helps maintain adherence to protocols and improves practices.
Adaptable strategies: The QIP strategies can be applied in various clinical settings to improve care.
Patient education: Nurses should educate patients on safe adhesive use to empower them in their own care.
Conclusion
The QIP at Rajagiri Hospital, Aluva (Kerala) successfully reduced the incidence of MARSI, improved nursing knowledge, and standardised adhesive use protocols. These outcomes demonstrate the critical role of structured training, adherence to updated practices, and continuous monitoring in improving patient safety and care quality. This initiative serves as a model for other healthcare facilities seeking to reduce MARSI and improve adhesive-related patient outcomes. Future initiatives should focus on ongoing training, protocol standardisation, and collaboration with product manufacturers to further minimise MARSI occurrences.
The success of this initiative underscores the necessity of ongoing training, adherence to updated practices, and systematic monitoring in enhancing patient safety and care quality. The outcomes of this project provide a robust foundation for future improvements in adhesive-related care and serve as a model for similar quality improvement initiatives in other healthcare settings. Continued focus on education, product innovation, and protocol standardization will be essential in further mitigating MARSI and ensuring optimal patient outcomes.
1. Kottner J, et al. Medical adhesive-related skin injuries: A systematic review. Int Wound J 2021; 18(2): 123-34 2. Drosdowsky MA, et al. Strategies to reduce the incidence of medical adhesive-related skin injuries in clinical practice. J Wound Care. 2020; 29 (5): 216-20
3. Earle S, et al. Impact of training on healthcare professionals’ knowledge and practice in adhesive use. Nurs Stand 2022; 36 (1): 45-52
4. Jones L, et al. The role of wound care specialists in reducing MARSI: A review of current practices. Wounds (UK) 2023; 19(1): 36-41
5. Houghton PE, et al. Prevention and management of medical adhesive-related skin injuries in hospitalized patients. Wound Care Canada 2021; 19 (2): 12-19
6. Sullivan J, et al. A study on the effectiveness of a standardized adhesive protocol in reducing MARSI in critical care settings. Crit Care Nurs Q. 2022; 45 (3): 215-23.
7. McNichol L, et al. Medical adhesive-related skin injuries: A global perspective on prevention, treatment, and outcomes. J Wound Ostomy Continence 2020; 47 (5): 465- 70
8. Beeckman D, et al. Best practice recommendations for the prevention of medical adhesive-related skin injuries. J Tissue Viability 2021; 30 (4): 245-51

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.